1. Malar rash
advertisement
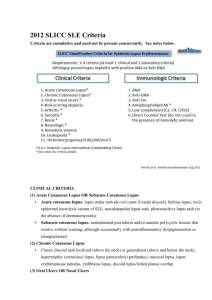
Systemic Lupus Erythermatosus(SLE) DR: DRGEHAN MOHAMED DR. GEHAN MOHAMED • Definition: chronic multisystem, autoimmune disease most commonly affecting young women. • any organ of the body may be involved . • course of the disease is remissions and exacerbations. • With good management, the ten years survival may be over 90%. Etiology and Pathogenesis of SLE A) Genetic factor • • • Certain genes permit a little immune overresponse, or presentation of high quantities of target antigens in certain tissues. Many studies have described familial aggregation of SLE. lupus have at least one first or second degree relative with lupus. B). Environmental factors 1. UltraViolet light, flares SLE in most patients .There is good evidence that exposure of skin to UV light alters the location and chemistry of DNA. 2. Drug-induced lupus. Drugs ( hydralazine, procainamide, beta-blokers, isoniazid, penicillamine) can induce lupus. Generally, lupus that is caused by a drug exposure goes away once the drug is stopped. 3. Infection: There has been continuing interest in the possibility that infectious agents might initiate or flare SLE. c) Sex hormones Female : Male 9 : 1 D)Abnormal immune system 1- molecular mimicry between external Ag and a self-Ag, 2- Defective regulatory mechanism. 3- nonspecific activation of T or B cells. 4- Autoantibodies to DNA, RNA:Circulating immune complexes (Ag &Ab complexes are frequently observed and these may deposit in the kidney, skin, brain, lung, and other tissues. It causes inflammation and tissue damage by a number of mechanisms, notably fixation and activation of the complement system which cause damage in the tissues. Clinical manifestations of SLE General symptoms The most common symptoms listed as initial complaints are fatigue, fever, and weight loss. • Fatigue Low grade fever, anemia, or any source of inflammation can result in fatigue. • Raynaud’s phenomenon it is commonly found in lupus. It lack specificity. (a triphasic reaction of distal digits to cold or emotion, in which the skin colour changes from white to blue to red) Dermatological involvement • • • • • Up to 85% of SLE Butterfly rash Maculopapular eruption Discoid lupus Relapsing nodular non-suppurative panniculitis • Purpuric lesions • Alopecia(loss of hair ) • Oral ulcer Malar rash: This is a "butterfly-shaped" red rash over the cheeks below the eyes and across the bridge of the nose. It may be a flat or a raised rash. The rashes are made worse by sun exposure Maculopapular eruption Discoid lupus These are red, raised patches with scaling of the overlying skin. Vasculitic skin lesin Alopecia Oral ulcer: • Painless sores in the nose or mouth . Musculoskeletal system • The arthritis of lupus is usually found on both sides of the body and does not cause deformity of the joints. Swelling and tenderness must be present. • The most frequently involved joints are those of the hand, wrists and knees,. • People with lupus can suffer from a certain type of low blood flow injury to a joint causing death of the bone in the joint. • The muscle involvement was reported in 30-50% of lupus patients Kidney system • Haematuria • Proteinure (>0.5g protein/day ) R.B.Cs Casts in urine Nervous system • The brain , nerve problems and psychiatric syndromes are common in lupus affecting up to two-thirds of people. • Potential disorders include seizures, nerve paralysis, severe depression, and even psychosis. • Spinal cord involvement in lupus is rare and occurs primarily when there is clot formation in a critical vessel that supplies blood to the spinal cord. Hematological abnormalities • Red blood cells a normochromic, normocytic anemia is frequently found in SLE. They appears to be related to chronic inflammation, drug-related, haemorrhage. haemolytic anemia due to presence of a serum antibody which attack red blood cells. • White blood cell leucopenia :its cause is probably a combination of destruction of white cells by autoantibodies, decreased marrow production, increased or marginal splenic pooling for W.B.Cs. it should also noted that the immunosuppressive drugs used in the treatment of SLE may cause a marked leucopenia. Vasculitis • Vasculitis in arteries throughout the body can account for signs and symptoms from a variety of organ involvements. Seen here is an artery with extensive vasculitis with chronic inflammatory cells. Pulmonary manifestations • Pleurisy: inflammation of the pleura • Pleural effusion: Pleural effusions may occur in SLE patients either due to direct pleural injury or secondary to nephrotic syndrome, infection, cardiac failure. Lung • 1) acute lupus pneumonia: • 2) pulmonary hemorrhage 3) chronic diffuse interstitial lung disease. the diagnosis should not be made until infectious processes such as viral pneumonia, tuberculosis, and other bacterial, fungal and pneumocystis carinii infection have been completely excluded. Cardiovascular manifestations • Pericarditis is the most common cardiac manifestation of SLE. • Myocarditis (Libman-Sacks endocarditis )and valvular disease • Hypertension, cardiac failure SLE can be associated with endocarditis. Shown here is Libman-Sacks endocarditis in which there are many flat, reddish-tan vegetations spreading over the mitral valve and chordae • . Gastrointestinal and hepatic manifestation • Esophagitis, dysphagia, nausea, vomiting: (drug related in most cases). • Chronic intestinal pseudo-obstruction, mesenteric vasculitis, protein-losing enteropathy. • Pancreatitis • Lupus hepatitis Eyes • The eyes are rarely involved in lupus except for the retina. Secondary sjogren’s syndrome • Dry eyes • Dry mouth exocrine glands were infiltrated with lymphocytes Secondary Antiphospholipid syndrome • characterized by recurrent arterial and /or venous thrombosis. Deep venous thrombosis • Notice the contrast between the involved left leg and the normal right leg. Redness, swelling, and warmth combined with discomfort in the involved leg are cardinal manifestations of a deep venous thrombosis. Diagnosis Criteria for diagnosing lupus • The diagnosis of lupus is a clinical one made by observing symptoms. Lab tests provide only a part of the picture. To receive the diagnosis of lupus, a person must have 4 or more of these criteria: Criteria for the diagnosis of SLE 1. Malar rash: Fixed erythema over malar areas 2. Discoid rash: Erythematous raised patches with keratotic scaling . 3. Photosensitivity: Skin rash after exposure to sunlight. 4. Oral ulcers: Oral or nasopharyngeal, painless. 5. Arthritis:Tenderness, swelling, effusion in 2 or more peripheral joints 6. Serositis: A) pleurisy or B) pericarditis 7. Renal disorder A) proteinuria >0.5g/24hour 8. Neurological disorder: A) seizures or B) psychiatric disorder. 9. Haematological disorder: A) haemolytic anaemia or B) leucopenia or C) thrombocytopenia 10. Immunologic disorder: A) positive LE cells or B) raised anti-native DNA antibdy binding or C) anti-Sm antibody 11. Positive antinuclear antibody Laboratory investigation Autoantibodies in SLE • Antibodies to cell nucleus component anti-DNA, antibodies to nuclear antigen (anti-Sm) • Antibodies to cytoplasmic antigens anti-SSA, anti-SSB • Cell-specific autoantibodies lymphocytotoxic antibodies, anti-neuron antibodies, anti-erythrocyte antibodies, anti-platelet antibodies • Antibodies to serum components antiphospholipid antibody Lupus band test • Immunofluorescence of skin with antibody to IgG demonstrates a band-like deposition of immune complexes that is bright green at the dermal epidermal junction in this skin biopsy taken from an area with a visible rash. With Systemic Lupus Erythermatosus such deposition can be found in both involved and uninvolved skin by a rash, whereas with Discoid Lupus Erythermatosus the immune complexes are found only in involved skin. Anti-nuclear antibodies • The lupus erythermatosus (LE) cell: Is a mature neutrophilic polymorphonuclear leukocyte, which has phagocytized a spherical, homogeneous-appearing inclusion, itself derived from nuclear material of degenerating leukocytes and coated with antinuclear antibody; a characterisitic of lupus erythematosus