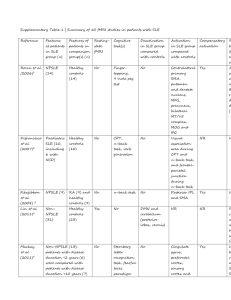
ACR vs SLICC Criteria for SLE Classification
advertisement
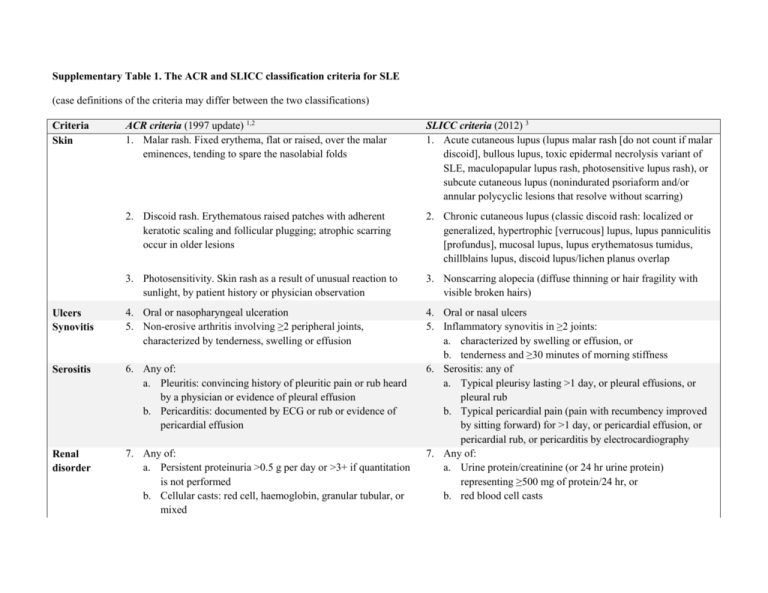
Supplementary Table 1. The ACR and SLICC classification criteria for SLE (case definitions of the criteria may differ between the two classifications) ACR criteria (1997 update) 1,2 1. Malar rash. Fixed erythema, flat or raised, over the malar eminences, tending to spare the nasolabial folds SLICC criteria (2012) 3 1. Acute cutaneous lupus (lupus malar rash [do not count if malar discoid], bullous lupus, toxic epidermal necrolysis variant of SLE, maculopapular lupus rash, photosensitive lupus rash), or subcute cutaneous lupus (nonindurated psoriaform and/or annular polycyclic lesions that resolve without scarring) 2. Discoid rash. Erythematous raised patches with adherent keratotic scaling and follicular plugging; atrophic scarring occur in older lesions 2. Chronic cutaneous lupus (classic discoid rash: localized or generalized, hypertrophic [verrucous] lupus, lupus panniculitis [profundus], mucosal lupus, lupus erythematosus tumidus, chillblains lupus, discoid lupus/lichen planus overlap 3. Photosensitivity. Skin rash as a result of unusual reaction to sunlight, by patient history or physician observation 3. Nonscarring alopecia (diffuse thinning or hair fragility with visible broken hairs) Ulcers Synovitis 4. Oral or nasopharyngeal ulceration 5. Non-erosive arthritis involving ≥2 peripheral joints, characterized by tenderness, swelling or effusion Serositis 6. Any of: a. Pleuritis: convincing history of pleuritic pain or rub heard by a physician or evidence of pleural effusion b. Pericarditis: documented by ECG or rub or evidence of pericardial effusion Renal disorder 7. Any of: a. Persistent proteinuria >0.5 g per day or >3+ if quantitation is not performed b. Cellular casts: red cell, haemoglobin, granular tubular, or mixed 4. Oral or nasal ulcers 5. Inflammatory synovitis in ≥2 joints: a. characterized by swelling or effusion, or b. tenderness and ≥30 minutes of morning stiffness 6. Serositis: any of a. Typical pleurisy lasting >1 day, or pleural effusions, or pleural rub b. Typical pericardial pain (pain with recumbency improved by sitting forward) for >1 day, or pericardial effusion, or pericardial rub, or pericarditis by electrocardiography 7. Any of: a. Urine protein/creatinine (or 24 hr urine protein) representing ≥500 mg of protein/24 hr, or b. red blood cell casts Criteria Skin Neurological disorder 8. Any of: a. Seizures: in the absence of offending drugs or known metabolic derangements b. Psychosis: in the absence of offending drugs or known metabolic derangements Haematologic 9. Any of: a. Haemolytic anemia with reticulocytosis disorder b. Lymphopenia: <1500/mm3 c. Thrombocytopenia: <100,000/mm3 Immunologic 10. Any of: a. Anti-DNA: antibody to native DNA in abnormal titer disorder b. Anti-Sm: presence of antibody to Sm nuclear antigen c. Positive finding of antiphospholipid antibodies based on: (1) an abnormal serum concentration of IgG or IgM anticardiolipin antibodies, (2) a positive test result for SLE anticoagulant, or (3) a false positive serologic test for syphilis known to be positive for ≥6 months and confirmed by Treponema pallidum immobilization or fluorescent treponemal antibody absorption test 11. Abnormal titer of ANA by immunofluorescence or an Antinuclear equivalent assay at any point in time and in the absence of antibody drugs known to be associated with “drug-induced SLE” syndrome Diagnosis of SLE At least 4 out of 11 criteria Abbreviations: ANA, antinuclear antibody; SLE systemic lupus erythematosus. 8. Any of: a. seizures, b. psychosis, c. mononeuritis multiplex, d. myelitis, e. peripheral or cranial neuropathy, f. cerebritis (acute confusional state) 9. Haemolytic anaemia 10. Leukopenia (<4000/mm3 at least once), or lymphopenia (<1000/mm3 at least once) 11. Thrombocytopenia (<100,000/mm3) at least once 12. Anti-dsDNA above laboratory reference range (except ELISA: twice above laboratory reference range) 13. Anti-Sm 14. Antiphospholipid antibody, lupus anticoagulant, false-positive test for syphilis, anticardiolipin (at least twice normal or medium-high titer), or anti-b2 glycoprotein 1 15. Low complement: low C3, or low C4, or low CH50 16. Direct Coombs test in the absence of haemolytic anaemia 17. ANA above laboratory reference range Either the biopsy-proven lupus nephritis in the presence of ANA or anti-dsDNA as a “stand alone” criterion, OR four criteria with at least one of the clinical and one of the immunologic/ANA criteria 1. Tan, E.M. et al. The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 25, 1271-7 (1982). 2. Hochberg, M.C. Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40, 1725 (1997). 3. Petri, M. et al. Derivation and validation of the Systemic Lupus International Collaborating Clinics classification criteria for systemic lupus erythematosus. Arthritis Rheum 64, 2677-86 (2012).