RESIDENTS.SLE
advertisement

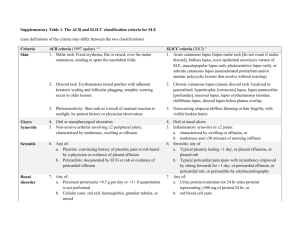
PEDIATRIC SYSTEMIC LUPUS ERYTHEMATOSUS Pediatric Rheumatology Red Team Resident Teaching Series Systemic Lupus Erythematosus • Episodic, heterogeneous, multisystem autoimmune disease – Widespread inflammation of vessels and connective tissues – Presence of antinuclear antibodies – Variable clinical manifestations and course – Incidence in adults: 2- 7.6 /100,000 per year • 18% have onset in childhood • Female to male ratio 8:1 Lupus in Children • • • • Uncommon before age 4 Incidence 0.5-0.6 /100,000 per year Females>males Children have more organ involvement than adults • Compliance issues in adolescence dangerous • Prognosis guarded; 30% may progress to renal insufficiency depending on treatment Current Theories Of Pathogenesis In SLE • • • • • • • • • • • Etiology unknown Multiple genes involved Immune dysregulation of B and T cell responses Immune complex deposition Abnormalities of complement Decreased clearance of apoptotic debris Hormonal imbalance Environmental triggers including UV B light, infection Loss of tolerance to chromatin and other autoantigens Cross reactivity between bacterial and mammalian DNA Abnormal response to DNA? These factors, acting alone or together, may trigger onset of disease in a genetically predisposed host. APOPTOSIS Protease (caspase) cascade Receptor ligation ex: TNF, Fas DNA fragmentation Chromatin condensation Cytoplasmic blebbing Clearance by phagocytes Y AUTOREACTIVITY Apoptotic bodies Y Immune complex disease • Antibodies can be against self (e.g. nuclear components in SLE) or foreign antigens (i.e. drugs or microorganisms in serum sickness) • Antibodies and antigens combine to form immune complexes • Immune complexes deposit in blood vessels and tissues and activate inflammatory response leading to tissue destruction Immune complex formation C’ Y RBC Y Endo BM Intima Complement fixation RBC Release of inflammatory, vasoactive and chemotactic mediators Disruption of endothelium C’ Y C’ Y C’ Thickening of BM Y Infiltration of inflammatory cells Tissue damage 1997 ACR CRITERIA FOR THE CLASSIFICATION OF SLE • Malar (butterfly) rash: – Fixed erythema, flat or raised, sparing the nasolabial folds • Discoid lupus rash: – Raised patches, adherent keratotic scaling, follicular plugging; may cause scarring • Photosensitivity: – Skin rash from sunlight • Oral or nasal mucocutaneous ulcerations: – Usually painless 1997 ACR CRITERIA FOR THE CLASSIFICATION OF SLE (cont) • Inflammatory arthritis: – Nonerosive, in two or more peripheral joints • Pleuritis or pericarditis • Cytopenias: – Hemolytic anemia, leukopenia (<4,000/mm3), lymphopenia (<1,500/mm3), or thrombocytopenia (<100,00/mm3) • Nephritis: – Proteinuria >0.5 gm/d – Cellular casts 1997 CRITERIA FOR THE CLASSIFICATION OF SLE (cont) • Encephalopathy: – Seizures – Psychosis • Positive ANA • Positive immunoserology: – Antibodies to dsDNA or – Antibodies to Sm nuclear antigen or – Positive findings of antiphospholipid antibodies based on: • anticardiolipin antibodies IgG or IgM, or • Lupus anticoagulant, or • False positive test for syphillis for at least 6 months (RPR/VDRL) Four of 11 criteria provide a sensitivity of 96% and a specificity of 100% in children Clinical Features of SLE • • • • • • • • Constitutional symptoms Musculoskeletal disease Mucocutaneous involvement Renal Disease Central nervous system disease Cardiopulmonary disease Hematologic abnormalities Gastrointestinal involvement Musculoskeletal Disease • Incidence: 76% – Arthralgias – Arthritis • Non-erosive • Involves small joints of the hands, wrists, elbows, shoulders, knees, ankles • Can be migratory, lasting 24-48 hours – Myalgias/ muscle weakness • Usually proximal Mucocutaneous Manifestations • Frequency: 76% – – – – – – – – – Malar rash Discoid lupus Vasculitis (purpura, petechiae) Raynaud’s phenomenon Nail involvement Alopecia Periungual erythema/ Livedo reticularis Photosensitivity Oral/ nasal ulcers Systemic lupus erythematosus: acute facial rash Acute malar rash Chronic facial rash Discoid lupus Discoid lupus alopecia photosensitivity Systemic lupus erythematosus: photosensitive erythematosus rash, upper back photosensitivity Oral ulcer Malar rash Systemic lupus erythematosus: palatal ulceration and malar rash Vasculitic ulcers Systemic lupus erythematosus: vasculitis, fingers Vasculitis: fingers Before treatment After treatment Systemic lupus erythematosus: vascultis, toes Raynaud’s Phenomenom Neuropsychiatric Manifestations Of SLE • Frequency: 20-40% • Difficult to diagnose and treat • Second to nephritis as most common cause of morbidity & mortality • Can occur at any time; even at presentation • Standard lab examinations have not been helpful in diagnosing or managing CNS sxs • Imaging modalities are not specific enough – SLE patients have imaging abnormalities but are clinically normal Neuropsychiatric Manifestations Of SLE • COMMON: Depression, organic brain syndrome, functional psychosis, headaches, seizures, cognitive impairment, dementia, coma • OCCASIONAL: Cerebral vascular accidents (thrombosis or vasculitis), aseptic meningitis, peripheral neuropathy, cranial nerve palsies • RARE: Paralysis, transverse myelopathy, chorea Diagnosis Of CNS Lupus • Cerebritis: CSF analysis shows pleocytosis; CT, MRI, MRA all may be normal or nonspecific • Autoantibodies (anti-neuronal, anticardiolipin, anti-ribosomal P) are not helpful • Vasculitis: CT, MRI, MRA may or may not be positive → conventional angiography • CVA: CT, MRI often positive • Spectamine (PET) scans positive in mild, acute, or old disease • Neurocognitive testing • Electroencephalography for seizures Cardiovascular Findings In SLE • Pericarditis • Myocarditis • Sterile valvular vegetations (rarely clinically significant except for risk of bacterial endocarditis) • Arrhythmias • Cor pulmonale • Vasculitis (small vessels) • Atherosclerosis/ Coronary Heart disease • Dyslipoproteinemias Pulmonary Findings In SLE • • • • • • • • Incidence: 5-67% May be subclinical (abnormal PFTs) Pleuritis Pleural effusion Pneumonitis Pulmonary hemorrhage Pulmonary hypertension Restrictive lung disease & diffusion defects most commonly observed abnormalities on PFTs GI INVOLVEMENT IN SLE • • • • • • Mild LFT elevation--not significant clinically--BUT NEED TO EXCLUDE AUTOIMMUNE HEPATITIS Colitis Mesenteric vasculitis Protein-losing enteropathy Pancreatitis Exudative ascites Hematologic Findings In SLE • Leukopenia, especially lymphopenia • Anemia – mild to moderate, common, due to chronic disease and mild hemolysis – severe, uncommon (5%), due to immune mediated hemolysis (Coombs +) • Thrombocytopenia – mild 100-150K, common due to immune mediated damage – severe <20K, uncommon (5-10%), immune mediated damage • Bone marrow suppression/arrest--very rare, due to antibodies against precursors Coagulopathy In SLE • Hypocoagulable states: – Anti-platelet antibodies--decreased numbers of platelets or decreased function (increased bleeding time) – Other platelet dysfunction and thrombocytopenia – Anti-clotting factor antibodies • Hypercoagulable states: – Antiphospholipid Antibody Syndrome (APS): more later – Protein C and S deficiencies • Thrombotic thrombocytopenic purpura Renal Findings In SLE Most common cause of morbidity & mortality • Glomerulonephritis – at least 75% • Microscopic or gross hematuria • Proteinuria, including nephrotic syndrome • Hypertension • Decreased GFR • Renal failure (up to 30-50% of children prior to 1980) • Renal biopsy predictive of potential for renal damage – ISN/ RPS classification with NIH activity and chronicity indices Laboratory Findings • Cytopenias (anemia, thrombocytopenia, leukopenia) • Elevated ESR, CRP, Immunoglobulins • Hypoalbuminemia • Proteinuria; RBCs, casts in urine • Decreased creatinine clearance • Low complement levels (C3/ C4) • Autoantibodies (ANA, APL, Coombs, antiplatelet Ab, rheumotoid factor, etc.) • (Immune complexes) Antinuclear Antibodies (ANA) • Sensitive but not specific, 95-98% pts positive • Against nuclear components of the cell • Titer specific- up to 10% of population have +ANA w/o disease; also see with infections, medications, malignancy • Subtypes: – dsDNA: high specificity for lupus (over 80%) – ENA (extractable nuclear antigen) = RNP/ Smith; RNP assoc w/ MCTD, Smith specific for SLE – Ro/ La (SS-a/ SS-b): neonatal lupus, Sjogren’s – Histone: drug induced lupus SLE - Treatment • MILD DISEASE: Rashes, arthralgias, leukopenia, anemia, arthritis, fever, fatigue – Treatment: NSAIDs, low dose corticosteroids (<60 mg/day), antimalarials (hydroxychloroquine), low dose methotrexate • MODERATE DISEASE: Mild disease + mild organ system involvement such as: mild pericarditis, pneumonitis, hemolytic anemia, thrombocytopenia, mild renal disease, mild CNS disease SLE - Treatment • MODERATE DISEASE (cont.): – Treatment: Prednisone 1-2 mg/kg/day, NSAIDS, Antimalarials, Low dose methotrexate, Azathioprine, MMF • SEVERE DISEASE: Severe, life-threatening organ system involvement – Treatment: High dose corticosteroids (2-3 mg/kg/day or pulse), Immunosuppressives (IV pulse Cyclophosphamide), Plasmapheresis, Anticoagulation where appropriate SPECIAL CONSIDERATIONS IN CHILDREN AND ADOLESCENTS • • • • Life-long burden of renal failure and (multiple) renal transplant(s) Steroid toxicity Immunosuppressive toxicity Infection risk different in children: – CMV, EBV – Bacterial infections, esp. strep – Fungal infections • Developmental age and psychosocial issues