Systemic Lupus
Erythematosus
INTRODUCTION
Systemic Lupus erythematosus
( SLE ) is a syndrome of unknown
aetiology most commonly affecting
young women. Virtually any organ
of the body may be involved .
Typically the course of the disease
is a series of remissions and
exacerbations.
With good management, the ten
years survival may be over 90%.
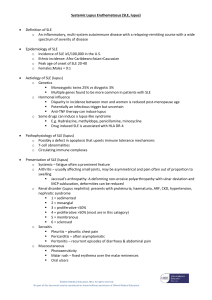
Etiology and Pathogenesis of SLE
1. Genetic factor
•
•
•
•
Many studies have described familial
aggregation of SLE. 5-13% of lupus
have at least one first or second degree
relative with lupus
It was found a 24-58% concordance in
monozygotic twins.
2-5% concordance in dizygotic twins or
siblings.
The risk of a child developing lupus born
from a mother (or father) with lupus is
calculated to be 3-4% at worst.
• What are the reasons of Genetic
susceptibility?
1. It seems likely that most of the genes predisposing to
SLE are normal.
2. An individual inherits an unlucky combination of
normal genetic polymorphisms, each of which
permit a little immune overreponse, or presentation
of high quantities of target antigens in certain tissues.
The combination of which is just enough to permit
SLE to evolve after some environmental stimulus.
3. C2, C4, C1q deficiencies, DR2, DR3, 1q41-42 region,
Fc-r RIIA, IL10 and Bcl polymorphisms.
2. Environmental factors
1.
2.
UV light, especially UVB, flares SLE in most patients.
It is unclear whether exposure to UV light can initiate
the lupus, but onset after a sunburn is not unusual.
There is good evidence that exposure of skin to UV
light alters the location and chemistry of DNA as well
as the availability of Ro and RNP antigens.
Drug-induced lupus. Drugs ( hydralazine,
procainamide, beta-blokers, isoniazid, penicillamine)
can induce lupus. Drug-induce lupus may resemble
SLE both clinically and serologically. Usually the
disease is mild, and renal and neurological
complications are rare. Generally, lupus that is
caused by a drug exposure goes away once the drug
is stopped.
3. Allergy. Does it induce lupus flare? No direct
evidence.
4. Infection. There has been continuing interest in
the possibility that infectious agents might
initiate or flare SLE. Mechanism might include
molecular mimicry between external Ag and a
self-Ag, epitope spreading, nonspecific activation
of T or B cells. There has been recent interest in
EB, CMV and other virus.
3. Sex hormones
• Female : Male=9:1
• The sex difference is most prominent
during the female reproductive years.
• In mice, castrating females and /or
providing androgens or antiestrogens
protects from disease,whereas
castrating males and providing
estrogens accelerates and worsens
SLE.
• The metabolish of sex hormone is
abnormal in some lupus patients. Men
and women with lupus metabolized
testosterone more rapidly than normal,
and estrogenic metabolites of estradial
persist longer in women.
• Neuroendocrine system.
Hyperprolactinemia, abnormalities in
hypothalamic and/or pituitary function.
4. Abnormal immune system
• Sustained presence of autoantigens:
increased apoptosis , impaired clearance of
apoptosis
• Hyperactivity in B and T lymphocyte.
• Increased expression of surface molecules
participating in cell activation in both B- and
T-cell.
• Overproduction of IL-6 and IL-10
• Defective regulatory mechanism.
Autoimmine Diseases
Autoimmune diseases result from a break
down of self tolerance
Autoantibodies to DNA, RNA, and a host
of other cell nucleus antigens.
Circulating immune complexes are
frequently observed and these may deposit
in the kidney, skin, brain, lung, and other
tissues. It causes inflammation and tissue
damage by a number of mechanism,
notably fixation and activation of the
complement system.
Overview of the pathogenesis of SLE
Infection
UV light
Self Ag
External Ag
Skin cell
Genetic susceptibility
APC
T cell
T cell
IC
APC
Defective IC clearance
B cell
Ab
Target
SLE
Tissue damage occurs by:
• 1. The formation of
immune complexes (type
III hypersensitivity)
• 2. Antibody mediated
injury to blood cells (type
II hypersensitivity)
The mere presence of the
autoantibodies seen in
these disorders can not
be the sole cause of
these disorders as the
antigens for all these
antibodies should
normally be sequestered
inside cells and not
exposed the antibodies in
the extracellular
environment.
Clinical manifestations of SLE
In systemic lupus erythematosus all pathways lead to endogenous nucleic acids-mediated
production of interferon (IFNα).
Bertsias G K et al. Ann Rheum Dis 2010;69:1603-1611
©2010 by BMJ Publishing Group Ltd and European League Against Rheumatism
Clinical manifestations of SLE
The clinical spectrum of SLE is very
broad
It make SLE both fascinating but
potentially difficult to diagnose and
manage.
Disease course of systemic lupus erythematosus (SLE).
Bertsias G K et al. Ann Rheum Dis 2010;69:1603-1611
©2010 by BMJ Publishing Group Ltd and European League Against Rheumatism
General symptoms
•
The most common symptoms listed as
initial complaints are fatigue, fever, and
weight loss.
Fever: fever secondary to active disease was
recorded from 50% to 86%. No fever curve or
pattern is characteristic. It can be difficult, but
very important to distinguish the fever of SLE
from that caused by complicating infections.
• Fatigue is common in patients with
SLE, especially during periods of
disease activity. It is also often the only
symptom that remains after treatment of
acute flares.
Low grade fever, anemia, or any
source of inflammation can result in
fatigue.
• Raynaud’s
phenomenon is
commonly found in
lupus. It lack
specificity.
(a triphasic reaction of
distal digits to cold or
emotion, in which the
skin colour changes from
white to blue to red)
Dermatological involvement
•
•
•
•
•
•
•
•
•
•
Up to 85% of SLE
Butterfly rash
Maculopapular eruption
Discoid lupus
Relapsing nodular non-suppurative
panniculitis
Vasculitic skin lesin
Livedo reticularis
Purpuric lesions
Alopecia
Oral ulcer
Photosensitivity
sun poisoning rash
Skin clinical and pathology changes: a typical lupus skin rash seen in July 2003 (A) and in
September 2003 (B).
Gensburger D et al. Ann Rheum Dis 2005;64:153-155
©2005 by BMJ Publishing Group Ltd and European League Against Rheumatism
• Malar rash: This is a
"butterfly-shaped" red
rash over the cheeks
below the eyes and
across the bridge of the
nose. It may be a flat or
a raised rash.
The rashes are made
worse by sun exposure.
• Maculopapular
eruption
• Discoid lupus
These are red, raised
patches with scaling of
the overlying skin.
Seal’s facial scars are the result of discoid lupus
SLE
• Drug induced lupus
has been seen with
hydralizine,
procainamide,
isoniazid and Dpenicillamine*; all
usually remit when
the offending drug is
discontinued.
• Vasculitic skin lesin
• Alopecia
• Oral ulcer: Painless
sores in the nose or
mouth need to be
observed and
documented by a
doctor.
• Ulcerated
leukocytoclastic
vasculitis in SLE
53 yo BF with severe generalized weakness,
weight loss, and chronic psychosis
Alopecia
Malar rash
Arthritis
Psychosis
Musculoskeletal system
• The arthritis of lupus is usually found on
both sides of the body and does not cause
deformity of the joints. Swelling and
tenderness must be present.
• The most frequently involved joints are
those of the hand, knees, and wrists.
• People with lupus can suffer from a certain
type of low blood flow injury to a joint
causing death of the bone in the joint.
• The muscle involvement was reported in
30-50% of lupus patients
• Avacular
necrosis of bone.
It may be caused by
prednisone therapy
Kidney system
• Haematuria
• Proteinure (>0.5g protein/d or 3+ )
• Cast
Nervous system
• The brain , nerve problems and
psychiatric syndromes are
common in lupus affecting up to
two-thirds of people.
• Potential disorders include
seizures, nerve paralysis, severe
depression, and even psychosis.
• Spinal cord involvement in lupus is
rare and occurs primarily when
there is clot formation in a critical
vessel that supplies blood to the
spinal cord.
Hematological abnormalities
• Red blood cells
a normochromic, normocytic anemia is
frequently found in SLE. They appears to
be related to chronic inflammation, drugrelated haemorrhage.
haemolytic anemia as detected by the
Coombs’ test is the feature of SLE.
on rare occasion, a serum antibody may
be produced which impairs red cell
production.
• Platelets.
thrombocytopenia (<100*109/L) appears
to be mediated by anti-platelet antibodies
or/and anti-phospholipid antibodies.
• White blood cell
leucopenia (<4.0*109/L), its cause is
probably a combination of destruction of
white cells by autoantibodies, decreased
marrow production, increased or
marginal splenic pooling, and
complement activation.
it should also noted that the
immunosuppressive drugs used in the
treatment of SLE may cause a marked
leucopenia.
Pulmonary manifestations
• Pleurisy
it is the most common manifestation of
pulmonary involvement of SLE. The volume
of pleural effusions usually is small to
moderate and maybe unilateral or bilateral.
Large pleural effusion are uncommon. It
usually exudative in character.
Pleural effusions may also occur in SLE patients with
nephrotic syndrome, infection, cardiac failure.
• Lung
1) acute lupus pneumonitis: fever,
dyspnea, cough with scanty sputum,
hemoptysis, tachypnea and pleuritic
chest pain.
2) pulmonary hemorrhage
3) chronic diffuse interstitial lung
disease.
the diagnosis should not be made until infectious
processes such as viral pneumonia, tuberculosis,
and other bacterial, fungal and pneumocystis
carinii infection have been completely excluded.
Cardiovascular
manifestations
• Pericarditis is the most common cardiac
manifestation of SLE.
• Myocarditis (the clinical features of lupus
myocarditis resembles that of viral
myocarditis)
• Libman-Sacks endocarditis and valvular
disease
• Hypertension, cardiac failure
• Pericarditis
•
SLE can be associated with endocarditis.
Shown here is Libman-Sacks endocarditis in
which there are many flat, reddish-tan
vegetations spreading over the mitral valve
and chordae.
Transesophageal image of a mitral valve
with masses characteristic of LibmanSacks endocarditis.
Gastrointestinal and hepatic
manifestation
• Esophagitis, dysphagia, nausea, vomiting:
(drug related in most cases)
• Chronic intestinal pseudo-obstruction,
mesenteric vasculitis, protein-losing
enteropathy
• Pancreatitis
• Lupus hepatitis
Eyes
• The eyes are rarely involved in lupus
except for the retina. People with lupus
often have to be screened by an
ophthalmologist if they are taking the
antimalarial drugs chloroquine or
hydroxychloroquine
Secondary sjogren’s
syndrome
• Dry eyes
• Dry mouth
exocrine glands were infiltrated with
lymphocytes
Secondary
Antiphospholipid
syndrome
• Antiphospholipid
syndrome (APS) is
characterized by recurrent
arterial and /or venous
thrombosis, fetal loss and
thrombocytopenia. High
titer of Antiphospholipid
antibody can be found in
APS patients.
(A) Cutaneous necrosis of the legs.
Fiehn C et al. Ann Rheum Dis 2001;60:908-912
©2001 by BMJ Publishing Group Ltd and European League Against Rheumatism
• Deep venous thrombosis
(blood clot). Notice the
contrast between the
involved left leg and the
normal right leg.
Redness, swelling, and
warmth combined with
discomfort in the involved
leg are cardinal
manifestations of a deep
venous thrombosis.
Laboratory investigation
Autoantibodies in SLE
• Antibodies to cell nucleus component
ANA, anti-dsDNA, antibodies to extracellular
nuclear antigen (ENA, anti-Sm, anti-RNP, antiJo1)
• Antibodies to cytoplasmic antigens
anti-SSA, anti-SSB
• Cell-specific autoantibodies
lymphocytotoxic antibodies, anti-neurone
antibodies, anti-erythrocyte antibodies, antiplatelet antibodies
• Antibodies to serum components
antiphospholipid antibody
anticoagulants antiglobulin (rheumatoid factor)
Anti-nuclear antibodies
• The lupus
erythematosus (LE)
cell
it has been
superseded by the
ANA and anti-dsDNA
techniques.
• ANA is a screening
test
anti-Sm, anti-dsDNA
antibodies are lupus
specific
antoantibodies.
• This homogenous pattern
of diffuse bright green
staining of nuclei seen by
immunofluorescence
microscopy with a Hep2
cell substrate is called
homogenous, and is the
most common pattern
with autoimmune
diseases overall.
• This rim (peripheral )
pattern of linear bright
green staining around
the peripheral of nuclei
seen by
immunofluorescence
microscopy with a
Hep2 cell substrate .
• dsDNA
• Nucleolar pattern
• Speckled pattern
Scl70, SSA, SSB, Sm
• These little Crithidia
organisms have a small
kinetoplast between the
nucleus and the flagella
which glows bright green
under
immunofluorescence
microscopy, and is
indicative of anti-native
DNA antibody that is very
specific for SLE.
• Immu-blotting
method to detect
anti-Sm, RNP, SSA,
SSB, Jo1, Scl70 and
ribosomal P.
Antibodies in SLE
• Antinuclear Antibody (ANA)
• Anti-Native DNA Antibody (Anti-nDNA)
• Anti-Smith (Anti-Sm)
• Anti-Ribonucleoprotein Antibody (Anti-RNP)
• Anti-RO/SSA; Anti-LA/SSB
Antinuclear Antibody
(ANA)
• Most useful in SLE
• Sensitive but not specific for SLE
• Also seen in drug-induced lupus, RA,
scleroderma, chronic hepatitis
• Since non-specific for SLE other more
specific antibodies were sought
ANA: peripheral pattern
• If ANA titer is > 1:160,
and there is a
peripheral pattern, it
strongly suggests
SLE
Anti-nDNA Antibody
• More specific than ANA
• Antibodies to “native” double-stranded
DNA, a specific nuclear constituent that
functions as an autoantigen
• Occurs in ~70% of patients with SLE
• Is
for SLE
Anti-nDNA Antibody
• Used to confirm SLE in someone
suspected of having SLE who has a
positive ANA
• Virtually all patients with a positive AntinDNA antibody have a positive ANA
• Therefore, don’t order if patient has a
negative ANA
Anti-Sm Antibody
• Antibody to Smith (Sm) antigen
• Specific for SLE
• Present in only 30% of patients with SLE
(therefore not sensitive for SLE)
Lupus band test
• Immunofluorescence of skin
with antibody to IgG
demonstrates a band-like
deposition of immune
complexes that is bright green
at the dermal epidermal
junction in this skin biopsy
taken from an area with a
visible rash. With SLE such
deposition can be found in skin
uninvolved by a rash, whereas
with DLE the immune
complexes are found only in
involved skin.
Vasculitis
• Vasculitis in arteries
throughout the body
can account for signs
and symptoms from a
variety of organ
involvements. Seen
here is an artery with
extensive vasculitis
with chronic
inflammatory cells.
• SLE is associated
with a peculiar
periarteriolar
fibrosis in the
spleen, as shown
here.
Kidney biopsy
• WHO classification of lupus nephritis is
based on light, immunofluorescence,
and electron microscopic findings.
WHO classification of lupus nephritis
immunofluorence
Pattern
mesangial
peripheral
electron microscopy
mesangial
subendothelial
subepithelial
Ⅰnormal
0
0
0
0
+
0
0
ⅡA mesangial deposit
+
0
0
ⅡB mesangial hypercellularity
+
0
+
0
++
+
++
+
++
++
++
++
+
++
+
+
0
Ⅲ
focal segmental GN
+
Ⅳ diffuse GN
+
Ⅴ membranous GN
++
Semiquantitative assessment of activity and chronicity
• Active indicators
cellular proliferation, necrosis, karyorrhexis,
cellular crescents, wire loops, hyaline thrombi,
leukocytic infiltration, interstitial infiltration.
• Chronicity indicators
glomerular sclerosis, fibrous crescents,
interstitial fibrosis, tubular atrophy
Indicators are scored on a scale of 0 to 3,with necrosis,
karyorrhexis, and cellular crescents weighted two times. The
maximum of activity is 24, and the maximum of chronicity is 12.
Diagnosis
Criteria for diagnosing lupus
• The diagnosis of lupus is a clinical
one made by observing symptoms.
Lab tests provide only a part of the
picture. The American College of
Rheumatology has designated 11
criteria for diagnosis. To receive the
diagnosis of lupus, a person must
have 4 or more of these criteria:
Criteria of the ARA for the classification of SLE
1. Malar rash:
Fixed erythema over malar areas, sparing nasolabial folds
2. Discoid rash: Erythematous raised patches with keratotic scaling and follicular plugging
3. Photosensitivity: Skin rash after exposure to sunlight, history or physical exam
4. Oral ulcers: Oral or nasopharyngeal, painless, by physical exam
5. Arthritis:Tenderness, swelling, effusion in 2 or more peripheral joints
6. Serositis: A) pleuritis or B) pericarditis
7. Renal disorder A) proteinuria>0.5g/24hour or 3+ or B) cellular casts
8. Neurological disorder: A) seizures or B) psychiatric disorder (having excluded other
causes, e.g. drigs)
9. Haematological disorder: A) haemolytic anaemia or B) leucopenia or C)
thrombocytopenia
10. Immunologic disorder: A) positive LE cells or B) raised anti-native DNA antibdy
binding or C) anti-Sm antibody or D) false positive serological test for syphilis.
11. Positive antinuclear antibody:
Management and treatment
1. Monitoring the lupus patients
• It cannot be emphasized too strongly
that lupus is a disease requiring regular
and careful follow-up.
• Important initial advice should be given
about avoiding UV light, infections,
extreme stress or fatigue
• Laboratory test—blood test, ESR,
C3,IC, liver function tests and antidsDNA.
2. Grading clinical activity
• The highly variable nature of the
syndrome
• Evaluation of lupus activity is the base
or beginning of therapy.
• Non-life-threatening features such as
arthralgia, skin rash, RP, alopecia
• Severe complication such as renal,
cerebral and heart involvement.
SLE disease activity index (SLEDAI)
Clinical feature
seizure , psychosis , organ brain syndrome
visual disturbance, cranial nerve disorder
lupus headache, cerebrovascular accidents,
vasculitis
arthritis
myositis
urinary casts, hematuria, proteinure, pyuria
rash, alopecia, mucosal ulcers,
pleurisy, pericarditis
low complement, increased DNA binding
fever
thrombocytopenia, leucopenia
score
8
8
8
8
4
4
4
2
2
2
1
1
3. Clinical therapy
• There are four main groups drugs useful in
the treatment of lupus: the non-steroid antiinflammatory drugs, anti-malarials,
corticosteroid and cytotoxic drugs.
• How to treat lupus is a kind of art. Which
and the dosage of drugs will be used to treat
the patient depend on lupus activity.
Treatment principles
• Depends on disease severity
• Fever, skin, musculoskeletal and serositis =
milder disease
• CNS and renal involvement – aggressive Rx
• Emergencies: - severe CNS involvement
- systemic vasculitis
- profound thrombocytopenia
(TTP-like syndrome)
- rapidly progressive nephritis
- diffuse alveolar hemorrhage
Medications used
•
•
•
•
•
•
•
•
Steroids
Cyclophosphamide
Azathioprine
Mycophenolate
Chloroquine
(Rituximab)
Plasma exchange/ IVIG
NSAIDS
Disease-modifying antirheumatic drugs
• Disease-modifying antirheumatic drugs
(DMARDs) are used preventively to reduce the incidence of
flares, the process of the disease, and lower the need for
steroid use; when flares occur, they are treated with
corticosteroids.
• DMARDs commonly in use are antimalarials and
immunosuppressants (e.g. methotrexate and azathioprine).
• Hydroxychloroquine is an FDA-approved antimalarial used
for constitutional, cutaneous, and articular manifestations,
•
whereas cyclophosphamide is used for severe
glomerulonephritis or other organ-damaging complications.
Steroids in Lupus
Steroid responsive
•
•
•
•
•
•
Dermatitis (local)
Polyarthritis
Serositis
Vasculitis
Hematological
Glomerulonephritis
(most)
• Myelopathies
Steroid non-responsive
•
•
•
•
Thrombosis
Chronic renal damage
Hypertension
Steroid-induced
psychosis
• Infection
Preventive care
• Medication-related (steroid) complications (Ca,
vit D, bisphosphonates)
• Aggressive BP and lipid control
• Immunization (complement deficient)
• Stress-dose steroid protocols for patients on
maintenance corticosteroids (surgery/ infection)
• Avoid UV exposure
• Avoid estrogen therapies
• Avoid sulfa-containing medications
• Pregnancy planning
Mildly active
lupus
Category I
arthritis,
arthralgia,
myalgia,
fatigue,
mild
mucocutaneous
involvement,
low-grade fever,
mild serositis,
lupus headache
combination of NSAID and /
or
antimalarials(chloroquine,
hydroxychloroquine) . The
drug of choice is
hydroxychloroquine (200
mg BD for 3 months and
then 200 mg daily).
Prednisolone remain the
drugs of first choice to
control lupus activity.
Low dosage <=10mg/d can
be used therapy
(Prednisolone 0.3-0.5
mg/kg/day)
Category II (Moderate SLE)
high-grade fever,
toxaemia,
severe
mucocutaneous
manifestations,
marked
photosensitivity,
moderate to severe
serositis,
lupus pneumonitis,
mild to moderate
myocarditis,
mesangioproliferative
or minimal change
lupus nephritis,
haemolytic anaemia
and thrombocytopenia
prednisolone 1 mg/kg
orally per day High dose
of steroid must be continued
till disease activity is well
controlled that usually takes up
to 6 weeks when it should be
tapered off slowly over 6 to12
months. In a toxic appearing
patient, the administration of
intravenous pulse
methylprednisolone (15 mg/kg,
max. 1 g) over an hour for 3 or
5 consecutive days may
achieverapid control of lupus
activity.
A combination therapy consisting of
high-dose daily oral prednisolone
(40-60 mg/day) and intravenous
organ/life-threatening
features such as :
cyclophosphamide pulses (0.75
focal/diffuse
gm/m2, maximum of 1 g, over 1
proliferative
hour) is recommended.
glomerulonephritis with
or without
The cyclophosphamide pulses are
azotaemia/hypertension
given once a month for 6 months
lupus cerebritis with
by which time usually remission is
recurrent seizures,
achieved and then a aintenance
acute confusional state,
pulse is administered every 3
coma;
systemic necrotizing
months for a total of 2 years of
vasculitis such as one
cytotoxic therapy. Prednisolone is
causing peripheral
tapered off or reduced to a very
gangrene, GI bleeding
low dose i.e. 5-7.5 mg per day by
Category III (Severe
SLE)
or mononeuritis ultiplex
6 months.
Category IV (SLE
with
miscellaneous
features)
antiphospholipid
syndrome (recurrent DVT,
CVAs, recurrent foetal loss
etc.),
pure membranous lupus
nephritis, chronic
sclerosing lupus nephritis,
seizures without other
evidence of lupus activity,
behavioural disorders
without other serious
manifestations,
resistant
thrombocytopenia or
haemolytic anaemia
resistant thrombocytopenia or
haemolytic anaemia
Immunosuppressive therapy
does not play any significant role
in these conditions. Treatment of
antiphospholipid syndrome.
Heparin and warfarin should be
started simultaneously so as to
allow an overlap of about 5 days.
INR should be adjusted
between 3 and 4 on long-term
warfarin therapy. The duration of
warfarin therapy is life-long in
patients with recurrent venous
thrombosis.
For refractory thrombocytopenia,
danazol may be useful.
regimen for
induction of remission (the first
6 months), which is then
maintained with azathioprine 22.5 mg/kg/day for about 2 years.
Biological agents
Abatacept
Abetimus
Anakinra (IL-1 receptor
antagonist)
Atacicept (TACI-Ig)
Blocks CD28-mediated
costimulation
Blocks the production of antidsDNA antibodies
Blocks IL-1 signalling
Infliximab (anti-TNF)
Soluble TACI receptor that binds
to BLyS and APRIL Reduction in
B cells and immunoglobulin levels
Blocks TNF
Rituximab (anti-CD20 mAb)
Depletion of B cells
Tocilizumab (anti-IL-6 receptor
mAb)
Blocks IL-6
Treatment of SLE
Arthritis, arthralgias, myalgias:
1. NSAIDS,
2. anti-malarials (eg. Plaquenil),
3. Steroids-injections,
4. oral methotrexate
Photosensitivity, dermatitis
1. avoid Sun exposure
2. topical steroids
3. Plaquenil
Weight loss and fatigue
steroids
Abortion, fetal loss
1. ASA
2. immunosuppression
Thrombosis
anti-coagulants
Glomerulonephritis
1. steroids
2. pulse cytotoxics
3. mycophenylate mofetil
CNS disease
1. anti-coagulants for thrombosis
2. Steroids
3. and cytotoxics for vasculitis
Infarction (secondary to
vasculitis)
1. steroids
2. cytotoxics
3. prostacyclin
Cytopenias
steroids
Management of proliferative (class III–IV) lupus nephritis.39 Systemic lupus erythematosus
patients with proliferative nephritis may be stratified into those with moderate-to-severe
versus severe disease based on impairment of renal function (increase in serum creatinine
≥30% and/or proteinuria ≥3.0 g/day) and/or presence of adverse renal biopsy histological
findings (crescents and/or fibrinoid necrosis >25% of glomeruli, chronicity index >4 or
chronicity index >3 and activity index >10).
Bertsias G K et al. Ann Rheum Dis 2010;69:1603-1611
©2010 by BMJ Publishing Group Ltd and European League Against Rheumatism
Management of renal lupus based on our own current practice.
Ioannou Y , Isenberg D A Postgrad Med J 2002;78:599-606
Copyright © The Fellowship of Postgraduate Medicine. All rights reserved.
Other therapy
•
•
•
•
Plasma exchange
Intravenous Immunoglobulin
Stem cell transplantation
Immune therapy ( anti-IL10, anti-CD20,
and immune tolerance therapy)
SLE and pregnancy
• SLE has been stable for more than 1
year.
• Prednisone is no more than 10mg/d,
and cytotoxic drug has been stopped
for more than 6 moth.
SLE patients can plan to have a baby.
Case #1
• 30 yo female
with
polyarthritis,
fever,
malaise, and
malar rash
Lab Work-up
• CBC
• Direct Coomb’s
• Platelet Count
• Urinalysis
•
• Anemia in 60-70%
(usu. normo/normo;
hemolytic in 10%);
WBC in 50%
• Thrombocytopenia in
15-30%
• UA: RBCs; +/-casts;
proteinuria
Which of the following is the probable diagnosis:
A. Dermatomyositis
B. Scleroderma
C. Rheumatoid arthritis
D. Polyarteritis nodosa
E. SLE
Case #1
• 30 yo female
with
polyarthr
itis(1),
fever,
malaise, and
malar
rash(2)
Systemic Lupus Erythematosus
Lab Work-up
• CBC
• Direct Coomb’s
• Platelet Count
• Urinalysis
•
• Anemia (3) in 6070% (usu.
normo/normo;
hemolytic in 10%);
WBC in 50%
• Thrombocytopenia
• (3) in 15-30%
• UA: RBCs; +/-casts;
proteinuria(4)
Which of the following is the probable diagnosis:
A. Dermatomyositis
B. Scleroderma
C. Rheumatoid arthritis
D. Polyarteritis nodosa
E. SLE
• ANSWER: E
Case 2: History
• A 36-year-old female is seen for migratory
arthritis of 6 months’ duration. She also
reports some fatigue and a photosensitive
skin rash. ROS notes:
•
•
•
Patchy hair loss 4 months ago that regrew
Aphthous-like mouth ulcers every 4 to 6 weeks
A diagnosis of “walking pneumonia” made last
month based on symptoms of pleuritic chest
pain
Case 2: Objective Findings
• Pain with mild
synovitis over the
MCPs and PIPs
• Rash over her face,
legs, and trunk
• Hgb = 12.1; ESR = 33
• UA = 3+ protein
• ANA = 1:640 titer
Case 2: Question
• With this clinical history, what is the most
important thing to do now?
A. Start an NSAID for the joint pain
B. Start hydroxychloroquine to treat the rash and
prevent recurrent pleurisy
C. Fully evaluate her renal status and initiate
appropriate therapy
D. Start prednisone at 80 mg qd
Case 2: Answer
• C. Fully evaluate her renal status
•
•
Don’t Wait
Aggressively evaluate renal status if the
urinalysis is abnormal in SLE patients
Case 2: History
• A 36-year-old female is seen for migratory arthritis
months’ duration. She also reports some fatigue and a
photosensitive skin rash.(2)
(1) of 6
ROS notes:
•
Patchy hair loss 4 months ago that regrew
•
Aphthous-like
•
A diagnosis of “walking pneumonia” made last month based on
symptoms of
mouth ulcers(3) every 4 to 6 weeks
pleuritic (4)chest pain
• UA = 3+ protein(5)
• ANA = 1:640 titer(6)
Prognosis
• Benign to rapidly progressive
• Better for isolated skin + musculoskeletal disease vs
renal and CNS
• Death rate 3X age-comparable general population
Mortality
Nephritis (most within 5 yrs of symptoms)
Infectious (active SLE + Rx – most common)
CVS disease (50X more MI than other woman)
Malignancy (chronic inflammation + Rx)
Summary
• Autoimmune disorder
• Multiple
manifestations
• Aggressive
investigation and
treatment
• Continued
surveillance
AMERICAN COLLEGE OF RHEUMATOLOGY (ACR)
CRITERIA FOR DIAGNOSIS OF SLE
•
•
•
•
•
•
•
•
Serositis (Pleurisy, pericarditis)
Oral ulcers
Arthritis
Photosensitivity
Blood disorders (Leukopenia, thrombocytopenia)
Renal involvement
Antinuclear antibodies (ANA)
Immunologic phenomena [false-positive Rapid Plasma
Reagin (RPR)]
• Neurologic disorder
• Malar rash
• Discoid rash
Course and prognosis
• An episodic course is characteristic, with exacerbations and
complete remissions that may last for long periods. These
remissions may occur even in patients with renal disease.
• A chronic course is occasionally seen. Earlier estimates of the
mortality in SLE were exaggerated; 10-year survival rate is
about 90%. In most cases the pattern of the disease becomes
established in the first 10 years; if serious problems have not
developed in this time, they are unlikely to do so. The arthritis is
usually intermittent. Chronic progressive destruction of joints as
seen in RA and OA occurs rarely, but a few patients develop
deformities such as ulnar deviation.
Summary - Key symptoms
•
•
•
•
•
•
•
•
Arthralgia
Alopecia
Discoid lesions
Fever
Malar rash
Oral ulcer
Photosensitivity
Weight loss
Summary - Key signs
• A patient must have 4 or more of the following 11 criteria
to be classified as having SLE
- Malar rash
- Discoid rash
- Photosensitivity
- Oral ulcer
- Arthritis
- Serositis
- Renal disease
- Neurologic disease
- Hematologic disorders
- Immunologic abnormalities
- Positive antinuclear antibodies (ANA)
Summary - Key tests
•
•
•
•
•
ANA
Anti-dsDNA
Anti-Sm
Complement levels (especially C3)
False-positive test for syphilis
Summary – Key treatment
• Corticosteroids: Solu-Medrol, prednisone
• Immunosuppressive drugs: methotrexate
(MTX), azathioprine
• Antimalariais: hydroxychloroquine
• NSAIDs
Thank
you
very
much!