SYSTEMIC LUPUS
ERYTHEMATOSUS
Manal Al Mashaleh
SYSTEMIC LUPUS ERYTHEMATOSUS
Autoimmune multisystem disease
characterized by widespread
inflammation and production of
autoantibodies
This means wide spectrum of
presentations
EPIDEMIOLOGY
Age:peak 15-40 years but any age
can be affected
Sex :more women affected ,10:1
during childbearing age
Clinical features
General
Severe fatigue
Fever
Weight loss
Anorexia
Lymphadenopathy
Dermatological features
MALAR RASH
Fixed
erythema, flat or raised,
over the malar eminences
Tending to spare the nasolabial
folds
30-60 %
MALAR RASH
Photosensitivity
Rash over the sun exposed
areas.Face,neck and V
shaped area of chest.See
rash varies in severity
depending on
exposure.Less under the
orbit protected areas.
Discoid lupus
Erythematous hyper
pigmented margins and
flat scarred hypo
pigmented centers
This can be seen in SLE
and pure cutaneous
lupus
DISCOID RASH
Erythematous
raised
patches with adherent
keratotic scaling and
follicular plugging
Atrophic scarring may
occur in older lesions
Subacute Cutaneous Lupus
Acute Cutaneous: Malar Rash
Note Sparing of Nasolabial Folds
Chronic Cutaneous:Discoid
Note Scarring, Hyperpigmentation
Livedo Reticularis
SLE - VASCULOPATHY
Small vessel
vasculitis
Raynaud’s
phenomenon
Antiphospholipid
antibody
syndrome
Alopecia
Oral lesions of SLE
Erythema of hard
and soft palate,
papules ,vesicles
and petechiae
Erythematous rash
of the tongue.
Oral Ulcers
Oral or
nasopharyngeal
ulceration,
usually painless,
observed by
physician
SLE ARTHROPATHY
Non erosive arthritis
Hand may show
diffuse soft tissue
swelling,ulnar
deviation,swan neck
deformity,MCP
subluxation.
Musculoskeletal
Synovitis-90% patients, often the earliest
sign
Osteoporosis
From SLE itself and therapy (usually steroids)
Osteonecrosis (avascular necrosis)
Can occur with & without history of steroid
therapy
Ocular
Conjunctivitis
Photophobia
Monocular blindness
transient or permanent
Blurred vision
Cotton-Wool spots on retina
due to occlusion retinal blood vessels
Serositis
Pleuritis :
convincing history of pleuritic pain ,pleural
rub heard by a physician or evidence of
pleural effusion
or
Pericarditis:
documented by ECG ,pericardial rub or
evidence of pericardial effusion
Pulmonary
Pleuritis the most common 30% in
life time of SLE patient
Peumonitis, pulmonary embolism,
pulmonary hypertension
Pulmonary hemorrhage: 50 %
mortality with treatment
Cardiovascular
Pericarditis the most common
Aortic insufficiency the most
common valvular lesion
Endocarditis
antibiotic prophylaxis indicated for
dental and surgical procedures
Accelerated atherosclerosis with 10
times higher mortality from
myocardial infarction from age and
sex matched
Lupus - Endocarditis
Noninfective thrombotic endocarditis involving mitral valve in SLE.
Note nodular vegetations along line of closure and extending onto chordae tendineae
(libman_sacks syndrome).
Renal
50% of all lupus patients will have
kidney involvement during their life
of these, 50 % will have serious
kidney disease
Persistent
proteinuria greater than 0.5
grams per day or greater than 3+
Cellular casts--may be red cell, hemoglobin,
granular, tubular, or mixed
Impaired kidney function
Lupus nephritis predict out come
(prognosis)
Major cause of mortality
How does lupus damage the kidneys?
Autoantibodies are formed against
antigens in the glomerulus basement
membrane
Circulating immune complexes bind to
the basement membrane of the
glomeruli
These result in inflammation of the
glomeruli (glomerulonephritis)
How does lupus damage the
kidneys?
The basement membrane is damaged by the
inflammation
Appearance of protein, white and red blood
cells and ‘casts’ in the urine
Low albumin levels in the blood resulting in
leakage of fluid from the vessels into the
tissues (edema)
Accumulation of waste proteins (uremia)
Hypertension
Do I really need a biopsy?
Most likely - YES
Kidney biopsies are important to
dictate how to treat
predict how long to treat
predict the chance for kidney function recovery
The biopsy helps determine treatment
Inflammation can occur:
Diffuse
Focal
Types of Lupus Nephritis
6 classes based on a WHO classification
Class I (normal) mild
Class II (mesangial) mild
Class III (focal proliferative glomerulonephritis)
moderately severe
Class IV (diffuse proliferative glomerulonephritis) severe
Class V (membranous glomerulonephritis)
Class VI (glomerulosclerosis) irreversible changes
Neurological
Seizures & Psychosis
in the absence of offending drugs or known
metabolic derangements; e.g., uremia,
ketoacidosis, or electrolyte imbalance
Cranial nerve lesions
Gastrointestinal & Hepatic
Uncommon SLE manifestations
Severe abdominal pain syndromes in SLE often
indicate mesenteric vasculitis, resembling
medium vessel vasculitis (PAN)
Diverticulitis may be masked by steroids
Hepatic abnormalities more often due to therapy
than to SLE itself
Laboratory Findings
Complete blood count
Anemia
Leukopenia
Lymphopenia
Thrombocytopenia
Complete blood count
Hemolytic anemia--with reticulocytosis
Leukopenia :less than 4,000/mm total on 2
or more occasions
Lymphopenia: less than 1,500/mm on 2 or
more occasions
Thrombocytopenia: less than 100,000/mm,
in the absence of offending drugs
Immunological findings
ANA - 95-100%-sensitive but not
specific for SLE
Anti -ds DNA-specific(60%) for SLE,
but positive to other non lupus
conditions
4 RNA associated antibodies
Anti-Sm (Smith)
Anti Ro/SSA-antibody
Anti La/SSB-antibody
Anti-RNP
Antiphospholipid antibody
Lupus anticoagulant
Anti-B2 glycoprotein 1 AB
Anti-cardiolipin
Depressed serum complement
ESR , CRP
CXR
Pleural effusion and pleural thickening
Pericardial effusion,cardiomegaly
Lung infiltrate from infection,pulmonary
embolism,Peumonitis,Interstitial lung
disease or hemorrhage
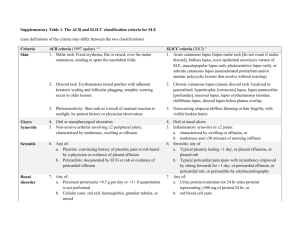
CLASSIFICATION
CRITERIA FOR CLASSIFICATION OF SLE
1.
2.
3.
4.
5.
6.
7.
8.
Malar rash
Discoid rash
Photosensitivity
Oral ulcers
Arthritis
Serositis
Renal disease.
Neurologic disease.
9. Hematologic
disorders:
-Hemolytic anemia
-Leukopenia
(Lymphopenia)
-Thrombocytopenia
10. Immunologic
abnormalities:
-Anti-ds- DNA
-Anti- Sm
-Antiphospholipid
-False +ve VDRL
11. Positive ANA
CLASSIFICATION CRITERIA
Must have 4 of 11 for Classification
Sensitivity 96%
Specificity 96%
Not all “Lupus” is SLE
Discoid Lupus
Drug induced lupus
Subacute Cutaneous Lupus
DIFFERENTIAL DIAGNOSIS
Rheumatic: RA, Sjogren’s
syndrome, systemic sclerosis,
dermatomyositis
Nonrheumatic: HIV, endocarditis,
viral infections, hematologic
malignancies, vasculitis, ITP, other
causes of nephritis
LUPUS RELATED SYNDROMES
Drug Induced Lupus
Classically associated with
hydralazine, isoniazid, procainamide
Male:Female ratio is equal
Nephritis and CNS abnormalities
rare
Normal complement and no antiDNA antibodies
Symptoms usually resolve with
stopping drug
LUPUS RELATED SYNDROMES
Antiphospholipid Syndrome (APS)
Hypercoagulability with recurrent thrombosis of either
venous or arterial circulation
Thrombocytopenia-common
Pregnancy complication-miscarriage in first trimester
Lifelong anticoagulation warfarin is currently
recommended for patients with serious complications
due to common recurrence of thrombosis
Antiphospholipid Antibodies
Primary when present without other SLE feature.
Secondary when usual SLE features present
SLE – treatment I.
Mild cases (mild skin or joint involvement):
NSAID, local treatment, hydroxy-chloroquine
Cases of intermediate severity (serositis,
cytopenia, marked skin or joint involvement):
corticosteroid , azathioprine, methotrexate
SLE – treatment II.
Severe, life-threatening organ involvements
(carditis, nephritis, systemic vasculitis, cerebral
manifestations):
high-dose intravenous corticosteroid + iv.
cyclophosphamide + in some cases:
plasmapheresis or iv. immunoglobulin, or,
instead of cyclophosphamide: mycophenolate
mofetil
Some cases of nephritis (especially
membranous), myositis, thrombocytopenia
cyclosporine
TREATMENT
Antiphospholipid Syndrome
Anticoagulation with warfarin (teratogenic)
subcutaneous heparin and aspirin is usual
approach in pregnancy
Lupus and Pregnancy
No longer “contraindicated”
No changes in therapy other than avoiding
fetal toxic drugs
Complications related to renal failure,
antiphospholipid antibodies
TREATMENT
ESR, CRP probably useful as
general markers of disease
activity
Complement and anti-DNA
antibodies may correlate to
disease activity
PROGNOSIS
Unpredictable course
10 year survival rates exceed 85%
Most SLE patients die from infection,
probably related to therapy which
suppresses immune system
Recommend smoking cessation, yearly
flu shots, pneumovax q5years