Case Study Presentation: LUPUS
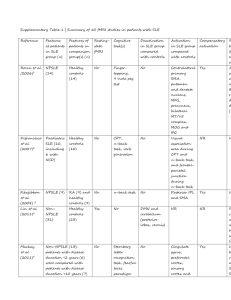
advertisement
https://www.youtube.com/watch?v=he RWz1Qmu4Q Listen to his words and accent Chronic, autoimmune disease that can affect literally any body system Rarely presents the same in any two lupus patients Disruption in apoptosis Immune system generates auto-antibodies › Antibodies clump together and can latch on to any body system. Attacking cells DNA surrounding the antibody. No known cause No know treatment to cure the disease › Treatment is aimed at reducing symptoms and balancing the body’s immune system to a functional level › Genetic, epigenetic, hormonal, and other environmental factors associated with SLE 250,000 Americans diagnosed with definite SLE (NADWG). 90% in women of childbearing age Incidence of SLE in black women 4x higher than that in white women D.W. Is a 25-year-old married woman with three children under 5 years old. She came to her physician 7 months ago with vague complaints of intermittent fatigue, joint pain, low-grade fever, and unintentional weight loss. Her physician noted small, patchy areas of vitiligo and scaly rash across her nose, cheeks, back, and chest. Positive antinuclear antibody(ANA) titer Positive dsDNA(positive lupus erythematosus) Positive anti-Sm(anti-smooth muscle antibody) Elevated C-reactive protein(CRP) Elevated erythrocyte sedimentation rate (ESR) Decreased C3 and C4 serum complement Joint x-ray films demonstrated joint swelling without joint erosion. D.W was subsequently diagnosed with systemic lupus erythematosus (SLE). She was initially treated with hydroxychloroquine (Plaquenil) 400mg and Deltason (Prednisone) 20mg PO qdaily, bed rest, and ice packs. › D.W responded well to treatment, the steroid was tapered and discontinued, and she was told she could report for follow-up every 6months, unless her symptoms became acute. D.W. Resumed her job in environmental services at a large geriatric facility. Positive antinuclear antibody (ANA) titer: › Auto-antibodies are in the immune system Positive dsDNA (positive lupus erythematosus): › Auto-antibodies that target DNA › Highly specific Positive anti-SM (smooth muscle antibody): › Presence of antibodies against smooth muscle Elevated C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) › Measure of inflammation in the body Decreased C3 and C4 serum complement › Shows impending or current “flare” of lupus symptoms 11 criteria for SLE › Established by the American Rheumatism Association › If individual display 4 or more of these criteria, SLE diagnosis is highly suggested. Known as a “butterfly” rash › D.W. displays scaly rash over cheeks, nose, back and chest. Discoid skin rash Photosensitivity Two or more swollen/tender joints › Shown both subjectively and objectively Brain irritation › Seizures or psychosis (lupus cerebritis) Mucous membrane ulcers Pleuritis or pericarditis Low blood counts Kidney abnormalities › Proteinuria Tests: › dsDNA, anti-Sm, ANA › ESR and CRP Coping and understanding of dx Monitor pain and temp Medication administration and understanding Ways to live a normal and safe life dx. w/ SLE Eighteen months after diagnosis, D.W. Seeks out her physician because of puffy hands and feet and increased fatigue. D.W. Reports that she has been working longer hours because of the absence of two of her fellow workers. Laboratory Test Results (8 months after dx): Sodium 129mmol/L Norm =135-145 Potassium 4.2mmol/L Norm=3.5-5.2 Chloride 119mmol/L Norm=96-106 Total CO2 21mmol/L Norm=20-29 BUN 34mg/dL Norm=8-20 Creatinine 2.6mg/dL Norm=0.6-1.1 Glucose 123mg/dL <140 Urinalysis 2+ protein 1+ RBCs Elevated BUN and Creatinine Proteinuria and hematuria Slightly elevated sodium and chloride Stabilize labs Decrease swelling and fatigue Medication adjustment Promote kidney function Decrease risk of infection 6) The physician orders cyclophosphamide (Cytoxan) 100mg/m2/day orally in two divided doses. D.W. Weighs 140 lbs and is 5ft, 4in tall. How much will she receive with each dose? cyclophosphamide (Cytoxan) › Aklylating agent used for immunosuppressant therapy › Used for D.W.’s worsening symptoms of SLE D.W. Is seen in the immunology clinic twice monthly during the next 3 months. Although her condition does not worsen, her BUN and creatinine remain elevated. While at work one afternoon, D.W. Beings to feel dizzy and develops a severe headache. She reports to her supervisor, who has her lie down. When D.W. Starts to become disoriented, her supervisor calls 911, and D.W. Is taken to the hospital. D.W. Is admitted for probable lupus cerebritis related to acute exacerbation of her disease. Seizures Decreased LOC Slurred speech PERRLA A&O Muscle tone Symmetry Seizure precautions Infection control › Standard precautions › IV antibiotics Close monitoring Neurological assessments 9) While caring for D.W., which of these care activities can be safely delegated to the NAP? (select all that apply): a: Measuring D.W.'s BP every 2hrs b: Assisting D.W. With personal hygiene measures c: Counseling D.W. On seizure safety precautions d: Assessing D.W.'s neurological status every 2hrs e: Emptying the urine collection device and measuring the output f: Monitoring D.W.'s BUN and creatinine levels A,b,e The physician orders pulse therapy with methylprednisolone (SoluMedrol) 125mg IV every 6 hours and plasmapheresis once daily. Increased risk of infection Change in VS N/V, bone marrow suppression, hair loss, lethargy Blood is taken out, plasma is filtered out, replaced with other fluids, and replaced back into the body. Plasma contains inflammatory antibodies and other immunologically active substances 12) D.W. Returns to the floor following plasmapheresis. The NAP reports to you D.W.'s vital signs. BP=86/43, HR=108, RR=18, Temp=97.2(36.2) You go in to assess D.W. And find that she is complaining of a headache and some dizziness. BP=86/43, HR=108, RR=18, Temp=97.2(36.2) › Hypotensive- from plasmapheresis › Dehydrated Stabilizing BP Hydrating Decrease dizziness and headache Stabilize temp Assessing neurological signs and VS › Keeping doctor aware of any complications Stable VS A&O x4 Decreased report of pain and swelling extremities Decrease in fatigue Decrease in inflammation Fight off infection 1) 2) 3) 4) 5) Medication regimen Coping Proper hygiene Self-care with SLE and kidney complications When to notify health care provider 16) You note that D.W.'s husband is visiting her this afternoon. You enter the room to as whether they have any questions. D.W.'s husband states, “I have tried to tell her that she cannot go back to work. Sure, we need the money, but the kids and I need her more. I’m afraid that this lupus has weakened her whole body and it will kill her if she goes back to work. Is that right?” How should you respond to his concerns? Main cause of SLE Treatments aimed at curing the disease rather than managing it › grasp further understanding for health care workers to take the best care possible for SLE patients Ramachandran, R. R., Sakhuja, V. V., Jha, V. V., Kohli, H. S., & Rathi, M. M. (2012). Plasmapheresis in systemic lupus erythematosus with thrombotic microangiopathy. Internal Medicine Journal, 42(6), 734. doi:10.1111/j.1445-5994.2012.02810.x Robinson, M., Sheets Cook, ,., & Currie, L. M. (2011). Systemic lupus erythematosus: A genetic review for advanced practice nurses. Journal Of The American Academy Of Nurse Practitioners, 23(12), 629-637. doi:10.1111/j.1745-7599.2011.00675.x Ferenkeh-Koroma, A. (2012). Systemic lupus erythematosus: nurse and patient education. Nursing Standard, 26(39), 49-57. Poole, J. L., Hare, K., Turner-Montez, S., Mendelson, C., & Skipper, B. (2014). Mothers With Chronic Disease: A Comparison of Parenting in Mothers With Systemic Sclerosis and Systemic Lupus Erythematosus. OTJR: Occupation, Participation & Health, 34(1), 1219. doi:10.3928/15394492-20131029-06 Christian Pagnoux, C. P. (2007). Plasma exchange for systemic lupus erythematosus. Transfusion and Apheresis Science , 187-192. Retrieved from http://vincentbourquin.files.wordpress.com/2009/12/pe-for-sle.pdf Kang, I., & Park, S. H. (2003). Infectious complications in SLE after immunosuppressive t herapies. Current opinion in rheumatology, 5, 528–534. Hari, P., & Srivastava, R. N. Pulse corticosteroid therapy with methylprednisolone or dexamethasone. Indian journal of pediatrics, 4, 557–560.