SP1 Lupus podocytopathy: lupus related or mere coincidence
advertisement
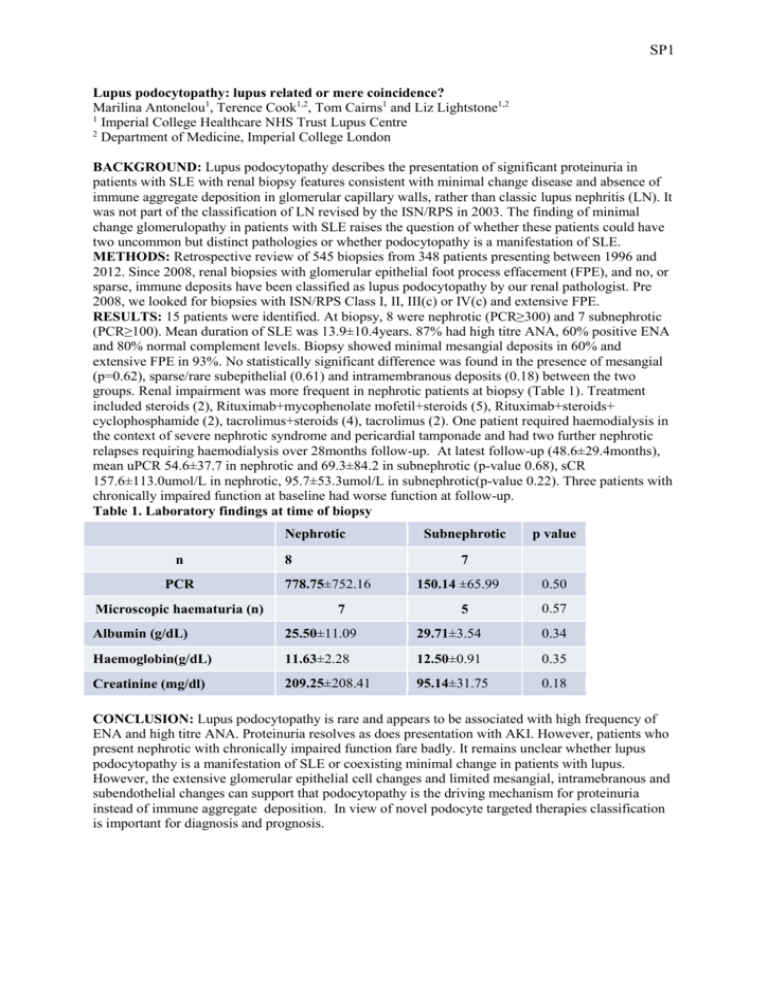
SP1 Lupus podocytopathy: lupus related or mere coincidence? Marilina Antonelou1, Terence Cook1,2, Tom Cairns1 and Liz Lightstone1,2 1 Imperial College Healthcare NHS Trust Lupus Centre 2 Department of Medicine, Imperial College London BACKGROUND: Lupus podocytopathy describes the presentation of significant proteinuria in patients with SLE with renal biopsy features consistent with minimal change disease and absence of immune aggregate deposition in glomerular capillary walls, rather than classic lupus nephritis (LN). It was not part of the classification of LN revised by the ISN/RPS in 2003. The finding of minimal change glomerulopathy in patients with SLE raises the question of whether these patients could have two uncommon but distinct pathologies or whether podocytopathy is a manifestation of SLE. METHODS: Retrospective review of 545 biopsies from 348 patients presenting between 1996 and 2012. Since 2008, renal biopsies with glomerular epithelial foot process effacement (FPE), and no, or sparse, immune deposits have been classified as lupus podocytopathy by our renal pathologist. Pre 2008, we looked for biopsies with ISN/RPS Class I, II, III(c) or IV(c) and extensive FPE. RESULTS: 15 patients were identified. At biopsy, 8 were nephrotic (PCR≥300) and 7 subnephrotic (PCR≥100). Mean duration of SLE was 13.9±10.4years. 87% had high titre ANA, 60% positive ENA and 80% normal complement levels. Biopsy showed minimal mesangial deposits in 60% and extensive FPE in 93%. No statistically significant difference was found in the presence of mesangial (p=0.62), sparse/rare subepithelial (0.61) and intramembranous deposits (0.18) between the two groups. Renal impairment was more frequent in nephrotic patients at biopsy (Table 1). Treatment included steroids (2), Rituximab+mycophenolate mofetil+steroids (5), Rituximab+steroids+ cyclophosphamide (2), tacrolimus+steroids (4), tacrolimus (2). One patient required haemodialysis in the context of severe nephrotic syndrome and pericardial tamponade and had two further nephrotic relapses requiring haemodialysis over 28months follow-up. At latest follow-up (48.6±29.4months), mean uPCR 54.6±37.7 in nephrotic and 69.3±84.2 in subnephrotic (p-value 0.68), sCR 157.6±113.0umol/L in nephrotic, 95.7±53.3umol/L in subnephrotic(p-value 0.22). Three patients with chronically impaired function at baseline had worse function at follow-up. Table 1. Laboratory findings at time of biopsy Nephrotic n PCR Microscopic haematuria (n) 8 Subnephrotic p value 7 778.75±752.16 7 150.14 ±65.99 5 0.50 0.57 Albumin (g/dL) 25.50±11.09 29.71±3.54 0.34 Haemoglobin(g/dL) 11.63±2.28 12.50±0.91 0.35 Creatinine (mg/dl) 209.25±208.41 95.14±31.75 0.18 CONCLUSION: Lupus podocytopathy is rare and appears to be associated with high frequency of ENA and high titre ANA. Proteinuria resolves as does presentation with AKI. However, patients who present nephrotic with chronically impaired function fare badly. It remains unclear whether lupus podocytopathy is a manifestation of SLE or coexisting minimal change in patients with lupus. However, the extensive glomerular epithelial cell changes and limited mesangial, intramebranous and subendothelial changes can support that podocytopathy is the driving mechanism for proteinuria instead of immune aggregate deposition. In view of novel podocyte targeted therapies classification is important for diagnosis and prognosis.