ELHDI – Lupus Overview – ENG
advertisement
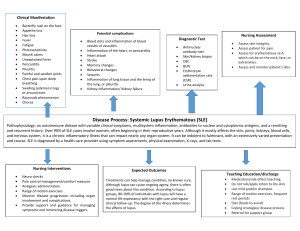
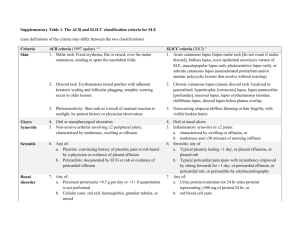
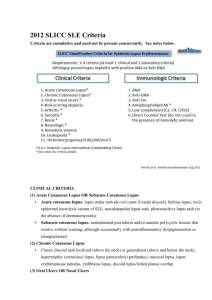
Get Into the Loop – Learn About Lupus Irene Blanco, MD, MS October 28, 2010 Cherkasky Auditorium, Montefiore Medical Center Agenda • Introduction to Lupus • Lupus and Your Heart – Dr. Mario Garcia • Question & Answer Session What is Lupus? • Autoimmune disease: • Excessive immune system activation • Loss of tolerance of immune system to one’s body • Certain genes are more likely to occur in patients with lupus • Many of these genes encode components of the immune system. • Abnormal estrogen metabolism • In animal studies estrogen worsens disease activity and causes early mortality Who Gets Lupus? • Female:Male ratio of 9:1 during childbearing years • Closer to 2:1 during childhood and after menopause, suggesting hormonal influence • Disease in males is can be more severe • 70% of SLE: females between ages 15-45 • 10% present age >60 Who Gets Lupus? • Highest occurrence is in Afro-Caribbean females 1:250 • African American to Caucasian ratio 3:1 • Child of SLE mother - risk of SLE 1:15 (7%) • 10-15% of SLE patients have 1st degree relative with SLE Mortality • 90% survive 5 years, 80% 10 years • Renal disease causes worse prognosis • African Americans have more aggressive and treatment resistant disease • Two different causes of death: – Early: disease activity and infections – Late: cardiovascular disease, disease activity, end stage renal disease, and thromboembolic Criteria for the Diagnosis of SLE • Malar (Butterfly) Rash • Discoid Rash • Sensitivity rash to the sun (Photosensitivity) • Ulcers in the nose and mouth • Arthritis • Fluid around the heart, lungs and in the abdomen • Lupus kidney disease • Neurologic Disorders: – Stroke, inflammation, depression, memory dysfunction, etc… • Anemia, low platelets and low white blood cell count • Abnormal blood antibody levels • ANA blood test Malar (Butterfly) Rash • Fixed red, flat or raised, over the bridge of the nose and cheeks • Tends to spare the nasolabial folds Discoid Rash • Red raised patches with scaling, skin follicle plugging • Can be very scarring • Singer Seal afflicted with discoid lupus at age 23 Photosensitivity • Skin rash as a result of unusual reaction to sunlight, by patient history or physician observation Oral and Nasal Ulcers • Oral or nasopharyngeal ulcers, usually painless Hair Thinning Arthritis • Non-erosive arthritis involving two or more joints, characterized by pain, swelling, or fluid collections • 80% of patients have it • Can move deformed fingers back into position • Pain may be out of proportion with appearance Severe or Life Threatening Complications Treatment of SLE Active Treatment • • Topical Steroids NSAIDs • Advil, Mobic, Naproxen • Steroids • Prednisone, Medrol • • Cytotoxics/Biologics • Cellcept, Cytoxan, Imuran, Benlysta Sunscreen • At least SPF 30 • Calcium, Vitamin D, Folate supplements • To help prevent SE from other medications Antimalarials • Plaquenil • Preventative Treatment • • Influenza Vaccine Pneumococcal Vaccine Side Effects to Lupus Medications • Weight gain • Hair loss, or new hair growth in unwanted places • Damage to the bones • Osteoporosis and Osteonecrosis • High blood pressure • High cholesterol • Low immune system and infections Follow Up Visits • How often depends on: – Lupus activity, severity, response to treatment, type of treatment, need for monitoring of medication side effects • At routine visits, blood and urine tests and should be checked • Even in patients with previously normal values • Patients with known kidney disease should also have urine checked every 8 weeks or so