Jaundice and Abnormal LFT`s
advertisement

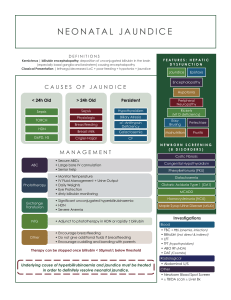
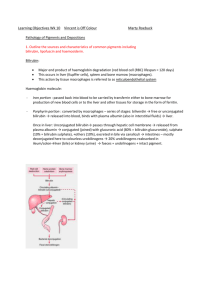
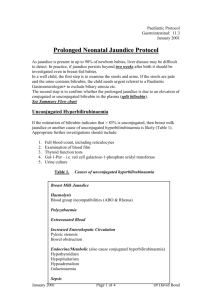
Jaundice Jaundice (icterus) refers to yellow pigmentation of skin, sclerae and mucosae due to increased plasma bilirubin visible at >35micromol/L Classified by site of problem (pre-hepatic, hepatocellular, post-hepatic) or by the type of circulating bilirubin (conjugated or unconjugated) Kernicterus is seen in infants with unconjuated hyperbilirubinaemia and involves deposition of jaundice in the basal ganglia, which can cause opisthotonus (state of a severe hyperextension and spasticity in which an individual's head, neck and spinal column enter into a complete "bridging" or "arching" position) Bilirubin metabolism Bilirubin is formed from the breakdown of haemoglobin. It is conjugated with glucuronic acid by hepatocytes, making it water soluble. Conjugated bilirubin is secreted into bile and passes out into the gut. Some is taken up by the liver again and the rest to converted to uribilinogen by gut bacteria. Urobilinogen is either reabsorbed and excreted by the kidneys, or converted to stercobilin which colours faeces brown. Pre-hepatic jaundice Increased bilirubin production – haemolysis, decreased liver uptale or decreased conjugation unconjugated bilirubin enters the blood As it is water insoluble, it does not enter urine resulting in unconjugated hyperbilirubinaemia Causes: physiological (neonatal), haemolysis, dyserythropoeisis (disorder in the production of red blood cells), Gilberts and Crigler-Najjar Syndromes Hepatocellular Jaundice Hepatocyte damage, usually with some cholestasis Causes: viral hepatitis (A,B,C, CMV, EBV), drugs (see table), alcoholic hepatitis, cirrhosis, liver mets/abscess, haemochromatosis, autoimmune hepatitis, septicaemia, leptospirosis, alpha-1-antitrypsin deficiency, Budd chiari, Wilson’s disease, Dubin Johnson and Rotor syndromes (failure to excrete conjugated bilirubin) Cholestatic (Obstructive) Jaundice If the common bile duct is blocked, conjugated bilirubin overspills into the blood causing conjugated hyperbilirubinaemia. Being water soluble, it is excreted in urine, making it dark. Less conjugated bilirubin enters the bowel, and the faeces become pale. When severe it can be associated with an intractable pruritus which is best treated by relief of the obstruction. Causes: common bile duct gallstones, pancreatic cancer (head of pancreas), lynph nodes at the porta hepatis, drugs (see Table), cholangiocarcinoma, PSC, PBC, biliary atresia, Mirrizi’s syndrome (obstruction secondary to compression of common hepatic duct by gallstone impacted in cystic duct) Clinical Features: Ask about – blood transfusions, IVDU, piercings/tattoos, sexual activity, travel, contacts, FH, alcohol, all medications Examine for: signs of chronic liver disease, hepatic encephalopathy, lymphadenopathy, hepatomegaly, splenomegaly, ascites, and palpable gall bladder (which in conjunction with painless jaundice suggests cause other than gallstones) Pale stools with dark urine = obstructive jaundice Tests: screening tests in suspected liver disease see below Urine – nilirubin is absent in pre-hepatic causes, urobilinogen is absent in posthepatic causes Haematology – FBC, Clotting, blood film, reticulocyte count, Coomb’s test Biochemistry – U+E, LFT (bili, ALT, AST, alk phos, GGT, total protein, albumin) USS – Are the bile ducts dilated >6mm (obstruction)? Are there gallstones, hepatic mets or a pancreatic mass? ERCP – if bile ducts are dilated and LFT not improving Perform a liver biopsy if bile ducts are normal Consider CT/MRI if abdominal malignancy suspected clinically NB Causes of Jaundice in a previously stable patient with Cirrhosis: Sepsis – especially from UTI, pneumonia Alcohol Drugs GI bleed Drug-Induced jaundice Haemolysis Hepatitis Cholestasis Antimalarials Dapsone Paracetamol overdose Anti-TB (r, I, p) Statins Sodium valproate MAOIs Halothane Antibiotics – fluclox, fusidic acid Anabolic steroids OCP Prochlorperazine Chlorpromazine Sulphonyureas Gold What is a Liver Screen? Tests for suspected liver diseases: VirusesEBV, CMV, Hep B and C serology Iron studies for haemochromatosis – raised ferritin and iron, low TIBC Alpha-1-antitrypsin deficiency Wilson’s disease – serum copper and caeruloplasmin reduced PBC – raised anti-mitochondrial antibodies PSC – raised ANA, AMA and ANCA may be +ve AIH – raised ANA and anti-smooth-muscle antibodies All immunoglobulins: raised IgA in alcoholic liver disease, IgG in AIH and IgM in PBC Hepactocellular carcinoma – raised alpha-feto-protein Conjugated and unconjugated bilirubin