Hyperbilirubinemia
advertisement

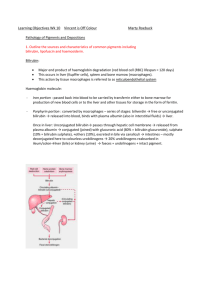
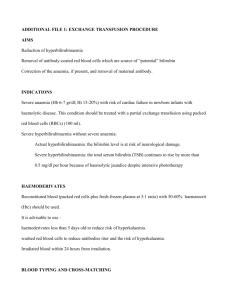
Hyperbilirubinemia Sara Pape-Salmon NP(F) VIHA, Mental Health & Addictions Services April 13, 2010 Demographics H.H. 64 year-old female Eastern European descent Resides in Victoria PMHx: Paranoid schizophrenia Obesity Over-flow incontinence likely PSHx: Tubal ligation Medications & Allergies: Loxapine 25 mg OD Multivitamin Folic Acid Vitamin B12 NKDA Social Hx: Lives alone No ETOH, currently non-smoker (remote 20 yr hx), no IVD/illicit drug use Receives intensive MHAS out-reach services Family hx is not known Chief Concern Serum icterus, slight (incidental finding) Fatigue? Lab Findings: Serum indices = slight icterus ALT, AST = normal Total bilirubin = high (29 umol/L) Conjugated bilirubin = normal (3 umol/L) ? Unconjugated bilirubin (was not obtained/tested) Dx & Pathophysiology Gilbert Syndrome Pathophysiology Most common inherited cause of unconjugated hyperbilirubinemia (recessive trait UGT1 gene) Underactivity of the conjugating enzyme system (diphospate glucuronyl transferase) Benign condition Physiology Review Bilirubin conjugation Bilirubin = byproduct of RBC destruction In plasma bilirubin binds to albumin & is lipid soluble = “unconjugated bilirubin” Unconjugated bilirubin can cross biologic membranes Physiology Continued Bilirubin conjugation cont: Unconjugated bilirubin moves into sinusoids in the hepatocyte & joins with glucuronic acid & becomes water soluble = “conjugated bilirubin” Conjugated bilirubin, now H2O soluble, can be excreted Excreted in urine (sm amt as urobininogen) and in feces (mostly) Signs & Symptoms Usually dx around puberty Often precipitated by intercurrent illness, dehydration, menstrual periods, stress, fasting states Abdominal cramps Fatigue Malaise Mild jaundice intermittently in some Many people are asymptomatic Differentials Hemolysis Hematoma Rhabdomyolysis Acute or chronic liver disease Infections Cardiac disease Medications (e.g. Atazanavir, probenicid, some antibiotics) Thyrotoxicosis Laboratory Studies CBC including retics and blood smear (exclude hemolysis, RBC abnormalities) Lactate dehydrogenase LFT’s Conjugated and unconjugated bilirubin Dx: Normal CBC, retic, blood smear, LFT’s, + unconjugated hyperbilirubinemia on several occasions, + absence of other disease process. Treatment Reassurance of benign nature Normal life expectancy No dietary or activity restrictions No medications for treatment References: McCance, K.L., & Huether, S.E. (2002). Pathophysiology: The biologic basis for disease in adults and children. (4th ed). Mosby Inc. St. Louis, Missouri. Mukherjee, S. (2009). Gilbert Syndrome. Found on-line at http://emedicine.medscape.com/article/176822overview.