Typical disorders of the liver 1. Secondary liver failure develops in a
advertisement
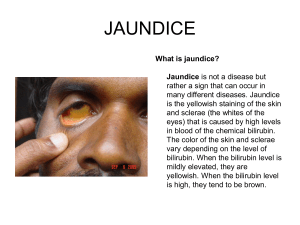
Typical disorders of the liver 1. Secondary liver failure develops in a) the action of carbon tetrachloride + b) circulatory failure c) phosphoric intoxication d) viral hepatitis e) Chronic alcohol intoxication 2. Primary liver failure develops in a) Heart Failure b) Shockt c) Renal insufficiency + d) viral infection of the liver e) diabetes mellitus 3. Manifestations of liver failure include: + a) Increasing the concentration of ammonia in the blood + b) Hypoproteinemia c) decrease in the activity of ALT and AST in the blood + d) Bleeding e) Dehydration 4. Violation of protein metabolism in hepatic failure are characterized by: a) hyperproteinemia; + b) hypoproteinemia; + c) hyperasotemia; + d) hypoprotrombinemia; + e) hyperaminoacidemia. 5. Accumulation of ammonia in hepatic failure especially toxic to a) the abdominal cavity; b) skin; c) muscles; d) bone; + e) of the central nervous system. 6. Disorders of carbohydrate metabolism in liver failure is characterized by + a) inhibition of gluconeogenesis; b) inhibition of the synthesis of ketone bodies; c) increased glycogen synthesis; d) increased conversion of galactose and fructose to glucose. 7. Disorders of lipid metabolism in hepatic failure are characterized by + a) a decrease in the formation of phospholipids; b) a decrease in the formation of ketone bodies; c) increased oxidation of fatty acids; d) an increase in the synthesis of high-density lipoprotein; e) increasing release of triglycerides from the liver to the intestine. 8. Hypocoagulation in hepatic failure is caused by: + a) malabsorption of vitamin K; + b) violation of the synthesis of fibrinogen; + c) violation of the synthesis of prothrombin; d) impaired synthesis of antithrombin III; e) violation of the synthesis of protein C and S. 9. Pathogenesis of hepatic coma significant dose: + a) Lack of neutralizing function of the liver + b) Metabolic acidosis + c) Lack ureaformation liver function d) Increase in blood direct bilirubin e) Hyperglycemia 10. Jaundice - is a) sickness; b) symptom; + c) syndrome; d) pathological reaction; e) pathological state. 11. Causes hemolytic jaundice include: + a) Action hemolitic poisons + b) Rhesus conflict between maternal and fetal body + c) incompatible blood transfusion d) hemorrhagic anemia e) gallbladder dyskinesia 12. Main link of the pathogenesis of hemolytic jaundice a) dehydration; b) heart failure; c) insulin deficiency; d) violation of the outflow of bile; + e) enhanced hemolysis. 13. Hemolytic jaundice is characterized by + a) increase in free bilirubin in the blood; b) increase of conjugated bilirubin in the blood; c) discoloration of feces; d) violation of digestion in the intestine; e) excretion of free bilirubin in the urine. 14. For hemolytic jaundice characterized by an increase in blood + a) indirect bilirubin b) direct bilirubin c) urobilin d) stercobilin e) bile acids 15. General pathogenesis obstructive jaundice is a) Damage to hepatocytes b) sialolithiasis c) Urolithiasis d) Reinforced hemolysis + e) Disturbance of the outflow of bile 16. Show causes of obstructive jaundice + a) Obturation hepatic and common bile duct b) hemolysis 17. Is observed in obstructive jaundice: + a) Hypotension + b) bilirubinuria + c) Acholia + d) Itching e) Tachycardia 18. Obstructive jaundice is characterized by an increase in blood a) biliverdin b) sterkobilinogen c) urobilinogen + d) direct bilirubin e) indirect bilirubin 19. Obstructive jaundice is characterized by: + a) hyperbilirubinemia; b) the increased activity of ALT and AST; + c) cholemia; + d) bilirubinuria; e) light urine. 20. Specify the changes in blood and urine when obstructive jaundice + a) cholemia, appearance of direct bilirubin in the blood, absence of urobilin in the urine; b) increase in indirect bilirubin in the blood, urobilin in the urine. 21. Syndrome of cholemia is caused by the pathogenic action of a) cholesterol; b) direct bilirubin; c) indirect bilirubin; d) fatty acids; + e) bile acids. 22. Cholemia is characterized by: + a) bradycardia; b) tachycardia. 23. Cholemia is characterized by: + a) lowering blood pressure; + b) appearance of skin itching; + c) bradycardia; d) tachycardia; e) hypertension. 24. The presence of bile salts in the blood causes a) increase in blood pressure; + b) bradycardia; c) tachycardia; d) increase in body temperature; e) shortness of breath. 25. Acholia - is the lack of bile a) in the blood; b) in the urine; + c) in the intestine; d) in the cerebrospinal fluid; e) in lymph. 26. For acholia is typical a) activation of the emulsification of fat in the intestine; b) hypervitaminosis of fat-soluble vitamins; c) increased cleavage and absorption of the fat; + d) steatorrhea; e) the dark color of feces. 27. Steatorrhea when obstructive jaundice is associated with + a) malabsorption of fats in the intestine; b) activation of pancreatic lipase; c) hereditary fermentopathy; d) activation of lipolysis; e) the development of primary malabsorption. 28. Bleeding during prolonged obstructive jaundice is caused by a) violation of the synthesis of heparin; + b) violation of the synthesis of prothrombin due to lower absorption of vitamin K; c) violation of the synthesis of inhibitors of fibrinolysis; d) violation of the synthesis of antithrombin; e) violation of the synthesis of kallikrein. 29. Parenchymal jaundice is characterized by: + a) urobilinogenemia; b) decrease in the activity of AST and ALT in the blood; + c) cholemia; d) hyperglycemia; + e) hypocholia. 30. Hyperbilirubinemia, which accompanied by increased levels of both free and conjugated bilirubin in the blood is observed at a) cholecystitis; b) sickle cell anemia; + c) Botkin's disease; d) cholangitis; e) insulinoma.