Workshop on jaundice..
advertisement

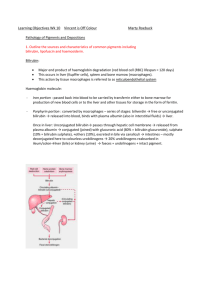
Workshop on jaundice Paul Lai Put down in your sheet a flow chart explaining the bilirubin metabolism Keywords: bilirubin, conjugation, urobilinogen, stercobilinogen, spleen, liver, terminal ileum, colon, kidney Put down in your sheet a flow chart explaining the bilirubin metabolism Urobilinogen absorbed into blood stream (get to the kidney and excreted in urine Unconjugated bilirubin from RBC destruction Conjugated bilirubin (in hepatocytes) Excretion into duodenum thro’ bile ducts Converted to Urobilinogen (in terminal ileum) Converted to Stercobilinogen (excreted in faeces) Urobilinogen absorbed into portal system and go back to liver Comparison between conjugated and unconjugated bilirubin • Unconjugated bilirubin • Conjugated bilirubin Comparison between conjugated and unconjugated bilirubin • Unconjugated bilirubin – Insoluble in blood – Largely attached to albumin in blood – Accumulates in pre-hepatic jaundice – Is toxic to tissues and organs such as the brain – Cannot be excreted in the urine • Conjugated bilirubin – Is water soluble – Small amounts are loosely bound to albumin in blood – Accumulates in posthepatic jaundice – Relatively non-toxic – Can be excreted in the urine What is the surgical significance of enterohepatic circulation of bile salts? What is the surgical significance of enterohepatic circulation of bile salts? • Primary bile salts help solubility of lipids allowing their absorption in the jejunum • After resection of terminal ileum (as in cases of right hemicolectomy for cancer), patient may have diarrhoea • Failure of resorption of bile acids may also lead to steatorrhoea Put down in your sheets the differential diagnosis of pre-hepatic, hepatic and post-hepatic jaundice • Pre-hepatic • Hepatic • Post-hepatic Put down in your sheets the differential diagnosis of pre-hepatic, hepatic and post-hepatic jaundice • Pre-hepatic – Haemolytic anaemia – Incompatible blood transfusion – Resorption of haematoma – spherocytosis • Hepatic – Cirrhosis of liver – Hepatitis – Drug and toxin reactions – Pre-maturity – Crigler-Najjer syndrome – Gilbert syndrome – DubinJohnson syndrome – Severe sepsis – SOL in the liver (mass effects by tumours or abscess) • Post-hepatic – Obstruction of extrahepatic bile duct due to gallstones / CBD stones/ Mirrizi syndrome – Strictures (primary sclerosing cholangitis, primary biliary cirrhosis, iatrogenic strictures) – Tumours (cholangiocarcinoma, ampullary cancer, pancreatic head cancer – Cholestasis (canaliculi obstruction) due to hepatitis, pregnancy, TPN, drug reactions It is wrong to simply classify jaundiced patients in having “medical jaundice” or “surgical jaundice” How to differentiate pre-hepatic, hepatic and posthepatic jaundice ? • Pre-hepatic • Hepatic in terms of 1. 2. 3. 4. 5. Color of urine Color of stool ALP level ALT level PT • Post-hepatic How to differentiate pre-hepatic, hepatic and posthepatic jaundice ? • Pre-hepatic – Urine of normal color – Stool of normal color – ALP normal – ALT normal – PT normal • Hepatic – Urine of dark color – Stool of normal color – ALP mildly raised (except in PBC) – ALT can be high if hepatitis or cirrhosis present – PT prolonged (and not correctable by vit. K) • Post-hepatic – Urine of dark color (but no urobilinogen) – Stool of pale color – ALP usually very high – ALT may be slightly raised – PT prolonged but correctable by vit. K Important details in the history in patients presenting with jaundice • • • • • • • • • • • • • • Duration of jaundice Previous attack of jaundice Any pain Any fever, chills and rigor Itchiness of skin (pruritus) Fat intolerance Exposure of drugs (including TCM) Systemic symptoms like weight loss, anorexia, general malaise Color of the sclera, urine and stool Contact with other jaundice patients History of hepatitis, IVDA, blood transfusions (especially transfusions long time ago) Occupations Alcohol consumption Family history of blood disorders, hepatitis or liver cancer Important details in the physical examination in patients presenting with jaundice • General examination – Depth of jaundice (Sclera, skin, mucus membrane) – Scratch marks – Stigmata of chronic liver diseases • • • • • • Abdominal examination – – – – – – • Palmar erythema Clubbing of fingers White nails Duputytren’s contracture Gynaecomastia Liver (size, shape, surface) If the gallbladder is palpable Splenomegaly Prominent abdominal wall veins Ascites Other abdominal masses Rarities – Kayser-Fleischer rings [Wilson’s disease] – Xanthmata [primary biliary cirrhosis] LFTs and USG • LFTs – Raised bilirubin in confirming the presence of jaundice – Raised enzymes (ALP / ALT) – Albumin (a low albumin level in a jaundice patient suggests chronic liver disease) – PT/APTT/INR (important to correlate clotting profile and liver functions) • *contribute to Child’s grading (bilirubin, albumin, PT) • USG – Almost always the first line of investigation – To look for dilated intrahepatic and extrahepatic bile ducts – Other things to pick up: • • • • Presence of gallstones and thickening of GB Presence of SOL or tumours (in the liver, porta hepatis, GB or pancreas) Presence of ascites Presence of splenomegaly and varices Cholangiograms • By endoscopic route: ERCP • By percutaneous route: PTBD • By MR imaging: MRCP • • By operative route: intra-operative cholangiogram Intravenous cholangiograms are almost obsolete these days • Always need to drain the biliary system (to relief obstruction) urgently if there are signs of acute cholangitis and septicaemia (septic shock) • Also needs to consider the invasiveness, availability of expertise & resources as well as the cost involved