IBD handout (Alex)
advertisement
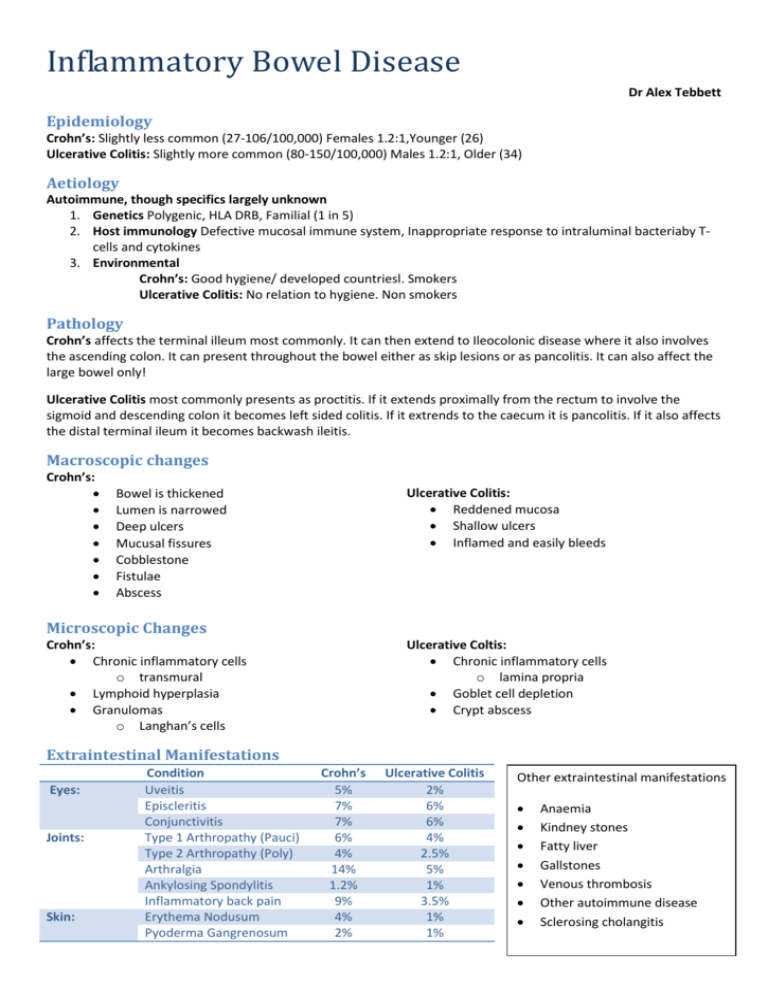
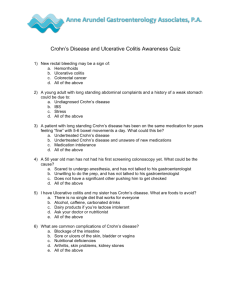
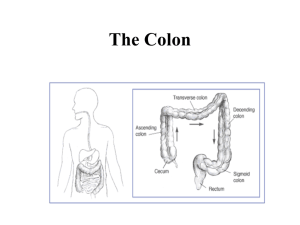
Inflammatory Bowel Disease Dr Alex Tebbett Epidemiology Crohn’s: Slightly less common (27-106/100,000) Females 1.2:1,Younger (26) Ulcerative Colitis: Slightly more common (80-150/100,000) Males 1.2:1, Older (34) Aetiology Autoimmune, though specifics largely unknown 1. Genetics Polygenic, HLA DRB, Familial (1 in 5) 2. Host immunology Defective mucosal immune system, Inappropriate response to intraluminal bacteriaby Tcells and cytokines 3. Environmental Crohn’s: Good hygiene/ developed countriesl. Smokers Ulcerative Colitis: No relation to hygiene. Non smokers Pathology Crohn’s affects the terminal illeum most commonly. It can then extend to Ileocolonic disease where it also involves the ascending colon. It can present throughout the bowel either as skip lesions or as pancolitis. It can also affect the large bowel only! Ulcerative Colitis most commonly presents as proctitis. If it extends proximally from the rectum to involve the sigmoid and descending colon it becomes left sided colitis. If it extrends to the caecum it is pancolitis. If it also affects the distal terminal ileum it becomes backwash ileitis. Macroscopic changes Crohn’s: Ulcerative Colitis: Reddened mucosa Shallow ulcers Inflamed and easily bleeds Bowel is thickened Lumen is narrowed Deep ulcers Mucusal fissures Cobblestone Fistulae Abscess Microscopic Changes Crohn’s: Chronic inflammatory cells o transmural Lymphoid hyperplasia Granulomas o Langhan’s cells Ulcerative Coltis: Chronic inflammatory cells o lamina propria Goblet cell depletion Crypt abscess Extraintestinal Manifestations Eyes: Joints: Skin: Condition Uveitis Episcleritis Conjunctivitis Type 1 Arthropathy (Pauci) Type 2 Arthropathy (Poly) Arthralgia Ankylosing Spondylitis Inflammatory back pain Erythema Nodusum Pyoderma Gangrenosum Crohn’s 5% 7% 7% 6% 4% 14% 1.2% 9% 4% 2% Ulcerative Colitis 2% 6% 6% 4% 2.5% 5% 1% 3.5% 1% 1% Other extraintestinal manifestations Anaemia Kindney stones Fatty liver Gallstones Venous thrombosis Other autoimmune disease Sclerosing cholangitis Differential Diagnosis Each other Infection (unlikely if >10 days) IBS Ileocolonic tuberculosis Lymphomas Treating IBD Induce remission Steroids – oral or IV Enteral nutrition Azathioprine / 6MP (Crohns) Maintain remission Aminosalicylates (UC) Azathipreine/ 6MP Methorexate Biologicals generally for Crohn’s only Infliximab, adalimumab Test for TB first! UC Flares: Truelove-Witts Criteria: 1. 2. 3. 4. 5. 6. Crohn’s 1. Azathioprine 2. Methotrexate 3. Cyclosporin 4. Humera Steroids for flares Ulcerative Colitis 1. Aminosalicylates 1. Mesalazie 2. Steroids 1. Foam/PR 2. Oral 3. IV 3. Azathiorprine (Acronym: A STATE) Anemia less than 10g/dl Stool frequency greater than 6 stools/day with blood Temperature greater than 37.5 Albumin less than 30g/L Tachycardia greater than 90bpm ESR greater than 30mm/hr Surgical Management Indications for surgery in Ulcerative Colitis Acute: Chronic o Failure Rx for 3 days o Poor Rx response o Toxic dilatation o Excessive steroid use o Haemorrhage o Non compliance Rx o Perforation o Risk of cancer (Acronym: I CHOP) Infection Carcinoma Haemorrhage Obstruction Perforation Prognosis UC 1/3 Single attack 1/3 Relapsing attacks 1/3 Progressively worsen requiring colectomy within 20 years Crohn’s Varied prognosis, new biological agents improving Cancer Both have increased risk of colon cancer, though UC>Crohn’s Screening colonoscopy done every 2 years after 10 years disease and every year after 20 years disease IBD for clinical finals Presenting complaint Crohn’s: Diarrhoea Abdominal pain Weight loss Malaise/lethagy Nausea/vomiting Low grade fever Anorexia Ulcerative Colitis Bloody diarrhoea Lower abdominal pain +/- mucus Malaise/lethargy Weight loss Apthous ulces in mouth What else to ask? Rashes Mouth ulcers Joint/back pain Eye problems Family history Smoking status Exploring their condition: Previous diagnosed? How many flares do they get? Are they well managed? Do they have any concerns about their treatment? Do they see a specialist? Examination General Exam Weight loss Apthous ulcer of mouth Anaemia Clubbing Abdominal Exam Colostomy bag May be some abdominal tenderness, may not. May find a RIF mass Abscess Inflamed loops of bowel Anything else? Rashes on the shins “I would also like to examine…” Anus Crohn’s: Odematous tags, fissures or abscesses Ulcerative colitis: usually normal PR Ulcerative colitis: blood Investigations Bedside Stool culture: exclude infection Sigmoidoscopy Bloods FBC : anaemia and likely raised WCC Haematemics: type of anaemia Inflammartory markers LFT: hypoalbuminaemia is present in severe disease, hepatic derrangement Blood cultures (if septicaemia is suspected) Serological: pANCA (UC) Imaging Plain AXR: helpful in acute attacks o Thumb printing/ Lead pipe sign Barium follow-through in Crohn’s CT CXR (Perforation) USS Special Tests Flexible sigmoidoscopy Colonoscopy o But never in severe attacks of UC due to high risk of perforation o May be painful in Crohn’s due to anal fissures o Diagnostic o Surveillance o UC of more than 10 years duration increased risk of dysplasia and carcinoma OGD o For Crohn’s: view of terminal illeum Management Manage the patient, not just the disease! Medications Manage extraintestinal manifestations o Eg B12 deficiency anaemia Manage patient’s symptoms o Eg loperamide for diarrhoea Good nutrition, hydration and vitamin supplements Psychosocial impact of disease o Ileostomy/colostomy bag o Flares and the need for a toilet Explanation Please explain a colonoscopy to the patient Please explain an OGD to the patient Please advise the patient on the side effects of steroids o Prepare an organised list to reel off, it is a very common question! Please explain the complications of inflixmab o Keep calm, remember it’s an immnuosupressent! How to do well in finals questions Have a plan on how to answer questions o Ix: bedside, bloods, imaging, special tests o Mx: medical, surgical, psychological, social acute and long term management Have a reason for each investigation you’d like to do Treat the person as well as the disease Don’t ever forget the MDT! What else could come up…. Coeliac disease IBS Ischaemic colitis Diverticular disease Appendicitis Polyps Haemorrhoids Know the side effects of steroids! Know the difference between colostomy and ileostomy! Clinical Scenario 29 year old female, one month history of loose watery stools, increasing in frequency to 12 time per day now. Occasionally stools have blood and slime mixed in with them. Cramping left iliac fossa pain. Feels unwell and lethargic. On examination, febrile at 38.2. Has a soft abdomen but slightly distended and tender in the left iliac fossa. PR examination is very painful and reveals fresh blood and mucus on the glove acute flare of ulcerative colitis Questions: What are your main differential diagnoses for this lady? How would you investigate this patient acutely and long term? Initial management in acute setting and the long term management? Can you compare the clinical presentation and pathological findings for Crohns and UC? Can you tell me the effect of smoking on UC and Crohns? What scoring system is used for acute UC? What are the extra-intestinal manifestations of IBD?