Inflammatory Bowel
Disease
Kevin Luey, FRACP
Gastroenterologist
Inflammatory Bowel Diseases
Infective colitis
Ulcerative colitis
Crohn’s colitis
Ischaemic colitis
NSAID-colitis
Radiation colitis
ULCERATIVE COLITIS
CROHN’S DISEASE
IBD
Chronic inflammatory disorders of
the gastrointestinal tract of
unknown aetiology but with an
autoimmune basis, characterised
by ulceration and inflammation of
the gut wall, causing abdominal
pain, diarrhoea and rectal
bleeding.
Prevalence
Prevalence varies world wide being more common in
developed countries. 100-200 per 100,000 in
western countries. ? Underestimate.
Higher prevalence in white races and Jews.
More common in close relatives.
The prevalence of Crohn’s in the NZ population is
approximately 100 per 100,000
Incidence
Was doubling every 10 years since 1940
Improved recognition
Appears to be increasing slowly now.
Real increase
Currently 10-20/100,000
Pathogenesis
Still unknown nearly 100 years after first
description
A combination of environmental factors
triggering chronic inflammation in a genetically
predisposed hosts.
Pathogenesis of IBD
genes
microflora
food
smoking
drugs
mucosal immunity
mucosal inflammation
IBD
Differences between Crohn’s and
UC
Differences in disease phenotype
Differences in genetic associations (e.g. IBD1 on
chromosome 16 coding for NOD2 important in
CD but not UC)
Both diseases long thought of as centering on
upregulated immune reactivity, but
increasing evidence of disordered innate immunity in
CD
Phenotype Differences between
Crohn’s disease and UC
Crohn’s Disease
Transmural
Small and large bowel
Skip lesions
Rectal Sparing
Granulomata common
Ulcerative Colitis
Mucosal
Large bowel only
Continuous disease
Rectal involvement 95%
Granulomata uncommon
Clinical presentations
and patterns of disease
IBD: key clinical factors.
Presentation
Natural History
diarrhoea, often bloody Onset any age, peaks early
adulthood and 40-60
abdominal pain
Relapse and remissions
weight loss
life-long
malaise
Ulcerative colitis
Clinical features
Unformed stools
Blood and mucus
Abdominal cramps
Urgency
Tenesmus
Disease distribution
Begins in rectum and extends
continuously proximally
UC Clinical course
Natural history
Fulminant (often first
episode)
Chronic relapsing and
remitting
Chronic continuous
Self limiting (<10%)
Relapse rate
50% in first year
Colectomy
Pancolitis 30-40% in 5 yrs
Distal colitis; 10% in 5 yrs
1%/year thereafter for all
These rates appear to be falling
since Infliximab has become
available
ASSESSING SEVERITY OF UC
(Truelove & Witts BMJ 1954)
mild
stools
<5/d, trace blood
temperature No fever
pulse
severe
>5/d, bloody
>37.8
<90
>90
Hb
Normal
<10.5
ESR
<30
>30
Crohn’s disease
Clinical features
Systemic symptoms
Due to chronic
inflammation
Lethargy
Loss of appetite
Weight loss
Fever
Intestinal symptoms
Depend on disease
distribution
Abdominal pain
Diarrhoea
Weight loss
Rectal bleeding
Nausea
Crohn’s disease
Sites of involvement
Small bowel
30%
Terminal ileum
80%
Small and large bowel
50%
Large bowel
20%
Diagnostic
investigations
Diagnosis
Stool culture
Blood tests
Endoscopy and histology
Radiology
Nuclear med scans
Inflammatory markers
Nutritional markers
White cell scans
DEXA
ASCA/ANCA
Faecal calprotectin
Blood tests
Raised CRP/ESR
Raised platelets: correlate well with IBD rather
than infectious colitis
Hypoalbuminaemia: correlates with high CRP
Full blood count – anaemia, neutrophilia
Iron, Vitamin B12, folate
Renal function
Liver function
Endoscopy
Oesophogastroduodenoscopy (gastroscopy)
Ileo-colonoscopy (colonoscopy)
Enteroscopy (small bowel)
Capsule endoscopy
Endoscopy (ILEO-colonoscopy)
Histology
Crypt distortion (implies inflammation for more
than 6 weeks)
Chronic inflammatory cells
Granuloma formation
Can help with diagnosing microscopic colitis
Radiology
Plain films
Contrast studies ? outdated
CT
Collections (e.g. abcesses)
Complications
US
Ba follow through, enema
Bowel wall thickening
Collections
MRI
Perianal disease
Small bowel
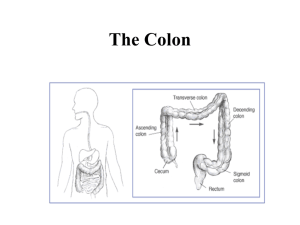
AXR IN ACUTE UC
Transverse colon
dilation, mucosal
islands and thumbprinting
Crohn’s disease
Ileal stricture: CT enteroclysis
Ileal stricture: MRI
Treatment strategies
MANAGEMENT OF IBD
General
Education - CCSG
Psychological support
Nutritional support
Avoid risk factors
smoking, drugs
‘MDT’
GP, physician, surgeon,
counsellor, nurse,
pharmacist, dietitian
Specific therapy
medical, surgical
Ulcerative colitis
Ulcerative colitis
goals of therapy
Induce remission
Maintain remission
Quality of life (IBDQ)
Prevent complications
Disease
Therapy related
Appropriate timing for surgery
Ulcerative colitis
Therapeutic considerations
Extent
Severity
Disease complications
Response to previous therapies
Lifestyle considerations
UC Treatment Options
5 ASA – topical / oral
Steroids – topical / oral / systemic
Azathioprine/6-MP/Methotrexate
Cyclosporine – oral / systemic
Immunological therapies - biologics
Surgery
Alternative therapies – e.g. Probiotics
No treatment entirely effective or safe
Management of fulminant colitis
mortality reduced from 50% - 1.5%
Meticulous clinical care
Multidisciplinary approach
IV hydrocortisone 100mg qds (60%)
Prophylaxis against DVT/PE
Cyclosporin 2mg/kg (levels 150-250)
60% initial response, 30% long term
? Biologics
Azathioprine on discharge
5 ASA for active UC
60% remission
OR 2.0 cf placebo in metaanalysis
Topical in left sided disease
(70% response)
Dose dependant
Renal toxicity
Dose dependant nephritis
Class effect
Which 5ASA? What dose
stomach jejunum ileum colon
Pentasa
(slow-release mesal)
Asacol, Salofalk
(pH-dependent mesalazine)
sulphasalazine, olsalazine, balsalazide
(azo-bonded)
CORTICOSTEROIDS IN IBD
Restrict to active IBD
No prophylactic role
Co-prescribe bone protection
Minimise long-term use
RESPONSE TO STEROIDS IN IBD
65% remission/improvement in 4/12
50% Crohn’s patients relapse or are steroiddependent at 1 year
`
PROBLEMS WITH STEROIDS
Given inappropriately
Recurrence after stopping
Side-effects
Failure to heal mucosa
SIDE-EFFECTS OF STEROIDS
osteoporosis - give calcium/vit D
diabetes
infections
osteonecrosis of hip
hypertension
glaucoma/cataracts
skin changes……….
Maintenance therapy for UC
5 ASA
Azathioprine
Biologics
Azathioprine
Long term maintenance strategy
Slow onset 2-3 months
Mainly uncontrolled data
36% 1 year relapse compared to 59%
??duration of therapy
Side effects of Azathioprine
Allergic responses
Leucopenia
Nausea and vomiting
Pancreatitis
Dermatological
? Malignancy
? Effects in pregnancy
Monitoring: regular FBC and LFT
Surgery for UC
Fulminant colitis
Failed medical treatment
Complications
Cancer risk
Surgery for UC
Panproctocolectomy
Ileostomy
Pouch formation
Close stoma
Crohn’s disease
Crohn’s disease
Goals of therapy
Similar to UC
Nutrition/growth
Surgery – Not curative
- High relapse rate
Fistula management
5ASA INDICATIONS
Crohn’s
mild-moderately active disease – esp. colon
? Effectiveness as maintenance
prophylaxis only after small bowel resection
Steroids in Crohn’s disease
Gut, 1994; 35: 360
Antibiotics in Crohn’s disease
Metronidazole
Perianal / colonic disease
?active disease
Some benefit post surgery 1yr
Neuropathy
Azathioprine as maintenance in
Crohn’s disease
Benefit at 2.5mg/kg but not much beyond
Methotrexate in Crohn’s disease
Start 25mg s/c weekly MTX for 16 weeks
Then maintain with 15mg s/c or oral weekly
Side effects of methotrexate
Allergic reaction
Folate deficiency
Oral ulceration
Bone marrow suppression
Pneumonitis/pulmonary fibrosis
Hepatic fibrosis
Teratogenic
Healing of Colonic Ulceration with
Anti-TNF Antibodies
Van Dullemen Gastroenterology 1995
Biologics
Anti- TNF alpha antibodies.
TNF alpha important near the beginning of the
inflammatory cascade
Blocking this prevents inflammation and
resultant ulceration etc.
Anti-TNF Antibodies
Binding Site for TNF
IgG
•Infliximab
•Chimeric monoclonal antibody
•Given as iv infusions (approx every 2 months)
•Adalimumab
•Fully humanised
•Given as subcut injection every 2 weeks
k
k
Infliximab Results
Chronic active
30% remission
30% improvement
Fistulation
Early recurrence on stopping
Concurrent immunosuppressives or
maintenance therapy essential
60% closure
General Contraindications
Intestinal sepsis
pregnancy, lactation (experience reassuring)
Infection – check esp. for TB
heart failure
malignancy
Side Effects
infusion reactions
acute 20%
delayed hypersensitivity 2%
ANA - 50% dsDNA Abs
lymphoma?
aplastic anaemia
heart failure
demyelination,
aseptic meningitis
infections
!!Cost - $5000 per infusion!!
Adalimumab
Humanised alpha TNF antibody
Therefore less immunogenic
Given subcutaneously rather than iv
Similar results to Infliximab
Same precautions and side effects
Given 2 weekly
COMPLICATIONS OF IBD
LOCAL
ulceration
bleeding
stricture
perforation
fistula
abscess
cancer
SYSTEMIC
eyes
joints
skin
liver
thrombosis
Extra-intestinal manifestations of
IBD
Erythema
nodosum
Pyoderma
gangrenosum
Colorectal Cancer in UC
High risk in Ulcerative Colitis
Very high risk if have sclerosing cholangitis
Risk increases with duration and extent of
disease
2% after 10 years
9% after 20 years
19% after 30 years
Colonoscopic Surveillance in UC
Recommended colonoscopic surveillance with
multiple biopsies
Every 2 years from 8-10 years after diagnosis
Annually after 20 years
High grade dysplasia – colectomy
Low grade dysplasia ? Colectomy
? 6 monthly colonoscopies
Colorectal Cancer in Crohn’s
Colitis
Evidence less clear cut than in UC
Increasing evidence that the risk is similar to UC
in Crohn’s colitis.
Most experts recommend same surveillance
programme as for UC
PROGNOSIS OF IBD
lifelong relapses and remissions
bowel resections
»
»
UC 20%
Crohn’s 70%
mortality increasing slightly in Crohn’s
mortality decreasing rapidly in UC
Time trends of death from ulcerative colitis (full line) and Crohn's disease (dashed lines).
Sonnenberg A Int. J. Epidemiol. 2007;36:890-899
Published by Oxford University Press on behalf of the International Epidemiological Association ©
The Author 2007; all rights reserved.
Summary
IBD common and affects wide range of age groups,
often the young
Multidisciplinary and holistic care is essential in such a
chronic condition
Treatment relies on induction of remission then
maintenance with anti-inflammatory and
immunosuppressive treatments
Steroids are not useful for maintenance
Immunosuppressive regimens are applied in a step-wise
approach
UNDERWRITERS’ VIEW
INCREASING PREVALENCE
DECREASING MORTALITY – Life ratings
MORE EFFECTIVE MEDICATIONS but
not without morbidity – probably balancing out
for TRB and Trauma (critical illness) ? For IP
BOWEL CANCER RISK LOWER THAN
PREVIOUSLY THOUGHT – Trauma and IP
Future genetic tests ?