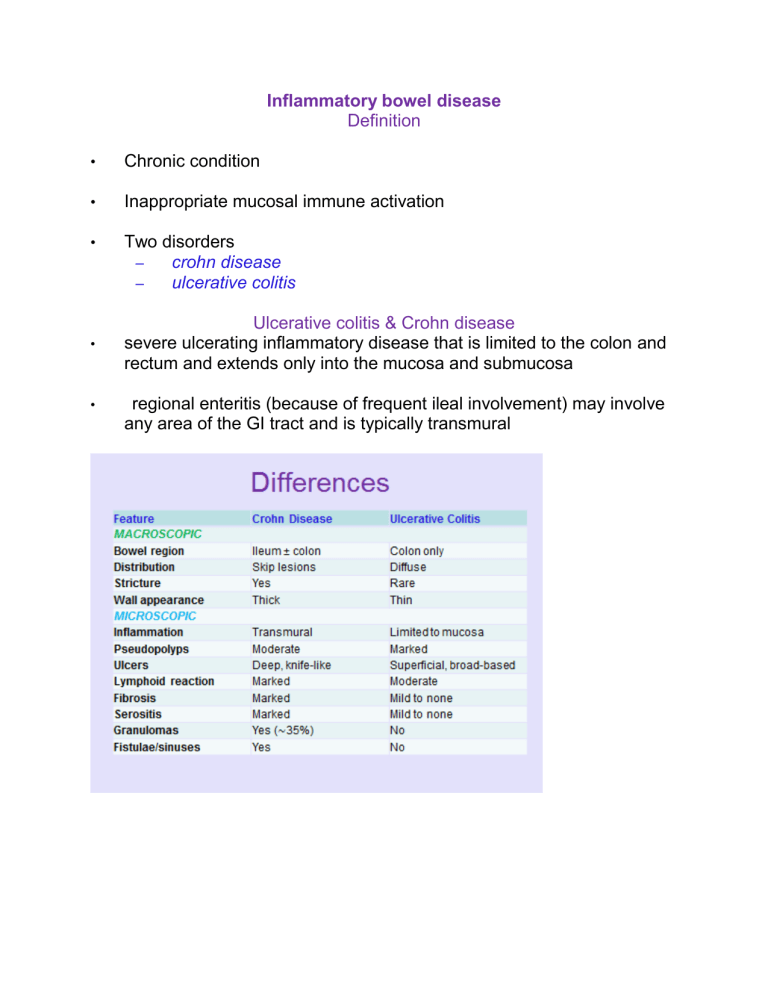
Ulcerative colitis & Crohn disease
•
•
•
•
•
Inflammatory bowel disease
Definition
Chronic condition
Inappropriate mucosal immune activation
Two disorders
– crohn disease
– ulcerative colitis
Ulcerative colitis & Crohn disease severe ulcerating inflammatory disease that is limited to the colon and rectum and extends only into the mucosa and submucosa
regional enteritis (because of frequent ileal involvement) may involve any area of the GI tract and is typically transmural
•
•
•
•
•
•
IBD
Teens and early 20s
Most common in north america, northern europe, and australia
IBD incidence worldwide is on the rise
Becoming more common in regions such as africa, south america, and
•
•
•
• asia, where the prevalence was historically low
* Hygiene hypothesis
Pathogenesis
idiopathic disorder combination of defects in host interactions with intestinal microbiota intestinal epithelial dysfunction
aberrant mucosal immune responses.
•
•
•
Genetics increased when there is an affected family member
> in crohn
NOD2 (nucleotide oligomerization binding domain 2) as a susceptibility gene in Crohn disease two Crohn disease –related genes ATG16L1 (autophagy-related 16-like)
& IRGM (immunity-related GTPase M
None associated with UC
•
•
•
•
•
•
•
•
• activated mucosal immunity and suppression of immunoregulation contribute to the development of ulcerative colitis and Crohn disease.
associated with
Mucosal immune responses defects in intestinal epithelial tight junction barrier function ( Crohn)
NOD2 polymorphisms
•
•
•
•
•
•
•
•
• defective transepithelial transport polymorphisms in ECM1 (extracellular matrix protein 1) (UC) defective epithelial anti-microbial function (paneth cell granule dysfunction)
Microbiota intestinal microbiota contribute to IBD pathogenesis antibodies against the bacterial protein flagellin are associated with
NOD2 polymorphisms (Crohn disease, but uncommon in ulcerative colitis ) probiotics, or beneficial bacteria may combat disease
Any area of GI
Crohn disease (granulomatous colitis) terminal ileum, ileocecal valve, and cecum
MC: limited to the small intestine alone in about 40% of cases multiple, separate, sharply delineated areas of disease (segmental distribution of the lesions skip lesions ) is characteristic aphthous ulcer cobblestone appearance
Fissures
Gross (Crohn) stricture formation creeping fat
•
•
•
•
•
Microscopic features
Patchy distribution distortion of mucosal architecture (crypt branching and budding)
Fissures, noncaseating sarcoid-like granulomas (present in 40 –60% of cases), and transmural involvement….the typical triad crypt abscesses ulcers (fissures) are linear, serpiginous (bear-claw or rose-thorn)
Clinical features. intermittent attacks of relatively mild diarrhea, fever, and abdominal pain bloody diarrhea
Relapsing and remitting disease cigarette smoking
Iron-deficiency anemia generalized nutrient malabsorption
•
•
•
•
•
•
•
•
•
•
•
•
•
Extra-intestinal manifestations of Crohn disease
Uveitis migratory polyarthritis
sacroiliitis
ankylosing spondylitis
erythema nodosum clubbing of the fingertips
Pericholangitis and primary sclerosing cholangitis occur in Crohn disease but are more common in ulcerative colitis
Complications
•
•
•
•
•
•
•
•
•
•
•
•
Fibrosing strictures
Perforations peritoneal abscesses risk of colonic adenocarcinoma is increased in patients with long-standing colonic disease intestinal disease is limited to the colon and rectum usually begins in the rectosigmoid area
In some cases, it remains localized to the rectum (
MC spreads proximally, sometimes to involve the entire colon
( pancolitis ) .
Ulcerative colitis ulcerative proctitis )
Gross broad-based ulcers (unlike serpiginous of CD) pseudopolyps wet and glaring from blood and mucus mural thickening is not present, the serosal surface is normal, and strictures do not occur
Normal mucosa
Abnormal
•
•
•
•
•
•
Histologic features
Architectural crypt distortion
The inflammatory process is diffuse, generally limited to the mucosa and superficial
Basal plasmacytosis
Mucosal and submocosa, the muscularis propria is rarely involved
Mucin depletion
Granulomas are not present in ulcerative colitis
•
•
•
•
•
Relapsing disorder
Attacks of bloody diarrhea with stringy, mucoid material
Lower abdominal pain
Clinical features.
Cramps that are temporarily relieved by defecation
Extraintestinal manifestations present
Complications
•
•
•
•
•
•
•
Perforation
Peritonitis
Abscess
Toxic megacolon
Venous thrombosis (most often in the iliac vein)
Carcinoma.
•
Colitis-associated neoplasia
• Risk increases sharply 8 to 10 years after disease initiation
Patients with pancolitis are at greater risk than those with only left-sided disease
Greater frequency and severity of active inflammation (characterized by the presence of neutrophils) may increase risk.
Dysplasia
-----------------The end----------------