The Colon - Neil Cronin
advertisement
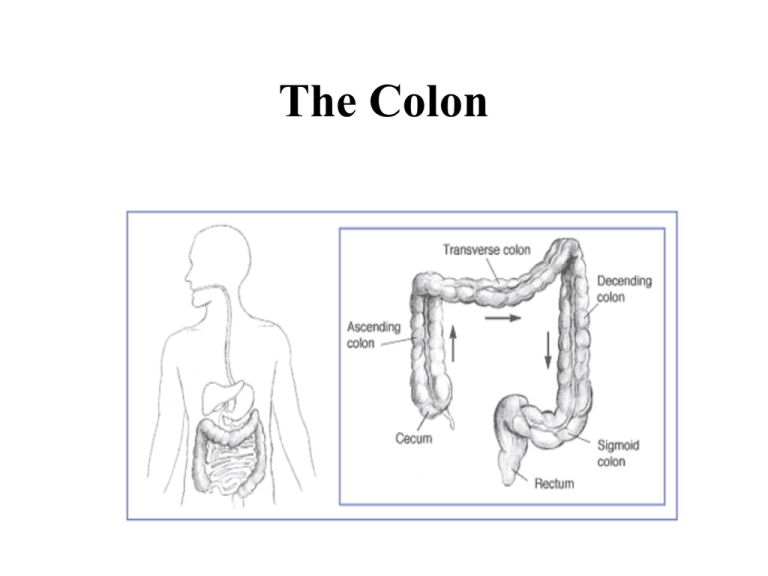
The Colon BLOOD SUPPLY OF THE COLON Physiological Function • Fluid re-absorption – reabsorbs 1.5-2 litres per day • Storage • Elimination • Enteric flora Symptoms & Signs in Colon Diseases Symptoms of Colonic Diseases • • • • • • • Diarrhoea Constipation Incontinence Flatulence Pain Blood per rectum Systemic symptoms ALARM SYMPTOMS • • • • • • Later age of onset Weight loss Anaemia Blood loss Nocturnal symptoms Family history colon cancer Origin of Abdominal Pain Intestinal structures Embryological origin Spinal segments Pain location Oesophagus, Foregut gastric, duodenal T5-6 to T8-9 Epigastric Small intestine to Midgut transverse colon T8-11 to L1 Peri-umbilical Transverse to recto-sigmoid T11 to L1 Suprapubic Hindgut Common causes of lower gastrointestinal bleeding • Anatomical – Diverticulosis • Vascular – Haemorrhoid – Angiodysplasia – Ischemic – Radiation-induced telangiectasia • Inflammatory – Infectious – Idiopathic inflammatory bowel disease • Neoplastic – Polyp – Carcinoma • Others – Ulcer – Post biopsy or polypectomy Vascular Ectasia Signs of Colonic Disease • • • • • Tenderness Rebound, guarding Mass Systemic signs Digital Rectal Examination Investigations • Radiology • Endoscopy Barium Enema Barium Enema Barium Enema Sigmoidoscopy Endoscopy Diseases of the Colon Diverticular Disease Diverticular Disease • Very common - >50% in over 50’s • 90% asymptomatic • Symptomatic >10% – Haemorrhage 25% sts massive – Diverticulitis 75% NATURAL HISTORY OF DIVERTICULAR DISEASE Symptomatic Simple Diverticular Disease • Colicky LIF pain • Constipation • STS rectal bleeding • Treatment: – Fibre – Stool softeners Complicated Diverticular Disease • Mucosal inflammation – diverticular colitis • Subserosal inflammation – diverticulitis – Abscess – Bleeding – Obstruction – Perforation/fistula ISCHEMIC COLITIS • • • • • Elderly arteriopaths CV risk factor profile Often after hypotensive episode Pain first, often mild Bleeding & diarrhoea BLOOD SUPPLY OF COLON Investigations • PFA – “thumb printing” • Endoscopy – rectal sparing – segmental involvement • CT scanning ISCHEMIC COLITIS Ischemic Colitis Management • • • • • Conservative approach iv fluids, treat anaemia Nutrition 10% later stricture Surgery for gangrene of colon C. difficile • Anaerobic gram-positive, spore-forming, toxinproducing bacillus 1935 • 1978 - c. diff identified as cause of antibiotic related diarrhoea – mostly clindamycin • fecal-oral route • Toxins A & B • Recently hypervirulent strain – 027 • Exponential increase RISK FACTORS – – – – – – – antibiotic use hygiene/handwashing hospitalisation/overcrowding advanced age PPIs GI surgery enteral feeding ANTIBIOTICS & CDAD Frequently associated Occasionally associated Rarely associated fluoroquinolones macrolides aminoglycosides clindamycin trimethoprim tetracyclines Penicillin (broad spectrum) cepalosporins sulphonamides chloramphenicol metronidazole vancomycin CLINICAL MANIFESTATIONS • • • • • Spectrum: asymptomatic to toxic megacolon Watery diarrhoea cardinal feature Offensive Often prominent systemic features Pseudomembranes on endoscopy MANAGEMENT • • • • • • • Stop antibiotics Infection control Supportive therapy Treat on suspicion Metronidazole or vancomycin Rarely surgery Relapses Inflammatory Bowel Disease • Ulcerative colitis • Crohn’s disease • Microscopic colitis – Lymphocytic colitis – Collagenous colitis Ulcerative Colitis • Ulcerative colitis is characterized by recurring episodes of inflammation limited to the mucosal layer of the colon. It almost invariably involves the rectum and may extend in a proximal and continuous fashion to involve other portions of the colon Crohn’s Disease Crohn's disease is characterized by transmural rather than superficial mucosal inflammation and by skip lesions rather than continuous disease. The transmural inflammatory nature of Crohn's disease can lead to stricture formation, microperforations and fistulae. Crohn's disease may involve the entire gastrointestinal tract from mouth to perianal area. Comparisons of various factors in Crohn's disease and ulcerative colitis Crohns UC rectum involved uncommom yes anus involved yes no TI involved often no colon involved often always PSC less common more commom Endoscopy Ulcers continuous Inflammation Transmural superficial Inflammation Skip continuous fistulae/stenoses Yes no Granulomas Often no Smoking increases risk lowers risk Surgical cure no yes Appendicectomy No influence protective Crohn’s Disease Crohn’s Disease Distribution of Crohn’s Disease Ulcerative Colitis Crohn’s Disease Ulcerative Colitis Crohn’s Disease Ulcerative Colitis Causes of Diarrhoea in Crohn’s Disease Consideration mucosal inflammation bacterial overgrowth bile salt diarrhoea bile acid deficiency lactase deficiency short bowel internal fistulae antibiotics (c. diff) Treatment anti-inflammatory Rx antibiotics cholestyramine low fat diet avoid latose low fat diet surgery treat Colon Carcinoma COLORECTAL CANCER • Polyp-dysplasia-cancer sequence – genetic – environmental Clinical Features – Depends on site of tumour – – – – – – – 1/3 proximal to splenic flexure Bleeding Change in bowel pattern Fe deficiency anaemia Pain non-specific Systemic features late Metastatic CLINICAL FEATURES • • • • • Abdominal pain — 44 percent Change in bowel habit — 43 percent Hematochezia or melena — 40 percent Weakness — 20 percent Anemia without other gastrointestinal symptoms — 11 percent • Weight loss — 6 percent Investigation • • • • Sigmoidoscopy/Colonoscopy Biopsy Barium studies CT scanning Colon Carcinoma Dukes classification Dukes A - limited to bowel wall Dukes B - extends thro’ muscle wall Dukes C - LN involvement - C1 & C2 Dukes D - outside bowel wall Treatment • Surgery • Chemotherapy • Radiotherapy Screening • To detect cancer at treatable stage • Age > 50 years • Targeted screening Screening • • • • Faecal occult blood Sigmoidoscopy Colonoscopy Virtual colonoscopy Colon Polyp Colon Polyp Virtual Colonoscopy Virtual Colonoscopy