DKA Case Study
advertisement

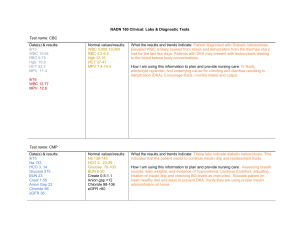
DKA Case Study Name:_Lindsey Gamrat John is an 18-year-old male with type I Diabetes. He is in the middle of his first semester of college. He has been brought to the ED by his roommate, who says that John began not feeling well while in their dorm room. John’s blood sugar is 1234, and the ED physician diagnoses him with DKA. John is admitted to the ICU. 1. Please describe three PHYSICAL and two LABORATORY findings you would expect to see in this patient. Provide rationale. This patient will likely be experiencing polyuria due to the increased blood glucose levels causing a hyperosmolar state in the body. Losing all of this fluid will lead to fluid volume deficit that will cause the patient to feel extremely thirsty (polydipsia). He may also have a fruity or metallic smelling breath. This is caused by the buildup of ketones in the body to a point where you can actually smell it on the patient’s breath. A laboratory finding in addition to elevated blood glucose could be elevated serum potassium. Insulin acts to move potassium out of the vasculature and in to the cells. A lack of insulin causes potassium to accumulate in the blood leading to hyperkalemia. An ABG would also reveal acidosis (pH less than 7.35). Ketone bodies are acidic and therefore an accumulation of them lowers the blood’s pH. 2. Identify three nursing diagnoses associated with John’s diagnosis of DKA. Provide rationale. One nursing diagnosis associated with DKA is fluid volume deficit. The hyperosmolar state of the body causes excessive diuresis. Patients in DKA can become very dehydrated. Fluid volume deficit can then lead in to another nursing diagnosis: decreased cardiac output. Low blood volume and potential arrhythmias caused by potassium shifts could cause the heart not to pump as effectively. Another nursing diagnosis that would follow decreased cardiac output is altered tissue perfusion. If the heart is not effectively pumping blood, tissues and organs are not getting enough of the oxygen rich blood they need to function. 3. Identify two nursing and two medical interventions that would be appropriate for John. Provide rationale. One of the most important nursing interventions for a patient in DKA is education. The patient needs to understand why the DKA occurred and what they can do to prevent it in the future. If they have been newly diagnosed with diabetes, they will likely need a lot of education not just on preventing DKA, but managing life with diabetes. The nurse also needs to encourage adequate food and fluid intake. As the hyperglycemia is treated, hypoglycemia actually becomes a concern. Adequate intake can help prevent this. The patient will also be extremely dehydrated so fluid intake is important. One of the main medical interventions will be to decrease blood glucose levels. This is usually done with IV insulin and most be done very slowly to avoid hypoglycemia and rapid shifts in potassium. In fact, when blood glucose is approaching desirable levels, IV dextrose is usually given with IV insulin to try and avoid hypoglycemia. Blood glucose levels will be very frequently monitored. The patient’s dehydration will also need to be treated so IV fluids in addition to the IV insulin will be given. Again it is important to monitor potassium and blood glucose closely. Additionally, the underlying cause of the DKA will need to be treated whether it be infection, illness, undiagnosed Type I diabetes or inadequate management of already diagnosed diabetes.