DKA - EPNO - Emergency Physicians of Northwest Ohio
advertisement

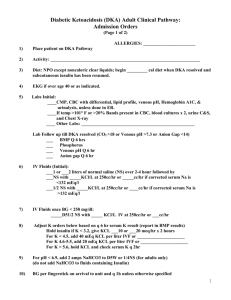
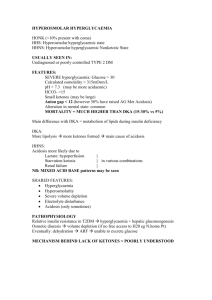
DKA: Management and Pitfalls Justin Bright, M.D. Emergency Physicians of NW Ohio February 20, 2013 Goals For Today • • • • • Definitions and characteristics of DKA Appropriate workup Treatment modalities Identify pitfalls and complications Discuss difference in adult vs. pediatric population • Management of DKA here at Henry Ford What Is DKA? • State of insulin deficiency (absolute or relative) causing dehydration, acidosis, and metabolic derangement • By blood work – Anion gap metabolic acidosis • • • • BHOB > 5 mEq/L Blood glucose > 250 mg/dL pH < 7.3 HCO3 < 18 mEq/L The Stats • • • • DKA is reason for 50% of diabetic admissions Tends to occur in patients less than 19 yo Type 1 DM > Type 2 DM Death occurs in 2% of presenting patients Causes of DKA? • • • • Underlying Infection (40%) Non-compliance with insulin regimen (25%) New onset diabetes (15%) Medical or surgical stress (20%) – AMI – Sepsis – “weak and dizzy” – Syncope – Altered mental status What Is Insulin? • Anabolic regulatory hormone • Released by pancreas (or administered as supplemental medication) in response to elevated blood sugar • Causes blood sugar to be utilized for fuel, with excess stored as muscle and fat • Inhibits release of glucagon • Inhibits gluconeogenesis and glycogenolysis Pathophysiology • Insulin deficiency • Hepatic gluconeogenesis and glycogenolysis • Fatty acid break down ketogenesis – Byproducts: ketones (acetone, BHOB, acetoacetate) • Excess blood glucose osmotic diuresis • BHOB induces vomiting more dehydration • Rising acidosis potassium shift and osmotic loss What Does DKA Look Like? • Insidious onset – Polydypsia, polyuria • Weakness, fatigue, malaise • Abdominal pain and vomiting as BOHB increases • Altered level of consciousness • May present with symptoms of their concurrent illness that triggered DKA A Case • 19 yo female in Room 115.5 • Known Hx of diabetes • CC: “One Touch Hi” • Reports being out of her insulin x 1 week • Mother reports patient is more confused and has been vomiting for 2 days What Do You Want To Know? ROS & PE • Review of Systems – – – – – Confusion Vomiting Frequent urination LMP 5 weeks ago Systems otherwise neg • Physical Exam – Tc 37.2, HR 115, BP 108/50, RR 28, SaO2 98 – Patient appears pale – Tachypneic, but not in distress – Poor skin turgor and capillary refill – No focal deficits, A/O x 3, but intermittently sleepy during questioning What Should We Order? • Diagnostics – – – – – – – – – – – One touch CBC Lytes UA, urine preg ABG w/ lactate Serum Osm B-Hob LFTs Lipase EKG ?? Imaging • Therapeutics – IVF Fluids (how much?) – Insulin (how much? Do you want to wait?) – Other meds? Labs Are Back! • • • • • • • • WBC 14 Na 126 Cl 92 HCO3 8 BUN 30 Cr 1.3 K 3.7 Glucose 786 • • • • • • • pH 7.12 CO2 23 Lactate 4.2 B-Hob 6.2 Osm 306 Gap 26 UA: large ketones and glucose • Ucg neg What Do You Think Of The Labs? • Na of 126 corrected 137 • K 3.7 (actually much lower intracellularly) • ABG anion gap metabolic acidosis with incomplete respiratory compensation • Acute kidney injury (pre-renal dehydration) • Lots of serum B-Hob persistent vomiting So Now What Do We Do? Treatment of DKA • • • • • ABC’s IV, O2, Monitor Fluids Insulin Correction of other electrolytes IV Fluids in DKA • Start with .9NS – If hypotensive rapid infusion of .9NS until SBP > 80 – If normotensive 1L of .9NS in first 30 minutes, another 1L within subsequent 1 hour • Change to ½ NS – Start at 250 cc/hr and titrate to urine output of 1-2 ml/kg/hr • Change to D5 ½ NS when blood sugar is < 250 but hydration still needed Saline vs. Ringers • Must really think about patient’s electrolyte status and composition of the fluids you’re giving • Normal Saline 154 mmol/L Na; 154 mmol/L Cl– Chloride can contribute to worsening acidosis – ½ NS has 77 mmol/L • Ringers 130 mmol/L Na; 109 mmol/L of Cl – Less Cl to contribute to acidosis – LR also promotes HCO3 formation helps further counter acidosis Insulin Administration • Use regular (Novalin) Insulin IV • Bolus of 10U IV prior to drip is controversial • Insulin Drip – 0.1 U/kg/hr • Stop the drip when blood glucose is 250 or lower • Goal drop in glucose is 50-100 per hr Electrolytes • Potassium – Need to watch the K levels!!!! – Patient’s are relatively K depleted – Insulin dramatically reduces K levels • Sodium – Remember that Na levels are deceptive because they are skewed by glucose levels • Bicarb – Use is controversial – Generally not indicated with pH > 7.0 – In peds patients use is associated with higher incidence of cerebral edema More on Potassium • Beware of the “warning colors” on Careplus • If K > 6 don’t give more • If K 4.5-6 consider 10 mEq infusion with fluids • If K 3-4.5 give 20 mEq infusion with fluids • If K < 3 give K before giving insulin Why Do DKA Patients Die? Because We Kill Them! How Do We Kill DKA Patients? • • • • • Cerebral Edema Poor ventilator management Not respecting the K levels Not monitoring glucose levels enough CHF from over-aggressive fluid administration Cerebral Edema in DKA • Occurs almost exclusively in patients < 20 yo • Mortality approaches 40% • Correlation with HCO3 administration – Causes paradoxical cerebral acidosis as lipid soluble CO2 crosses blood-brain barrier • Initial symptom is headache • Onset 12-24 hrs from treatment onset • Rapid deterioration of mental status What Do You About It? • • • • Manage airway Immediate head CT Neurosurg consult Do whatever you can to prevent herniation – mannitol • Pray! Ventilator Management • Must communicate with the RT about vent settings! • Keep in mind patient’s metabolic status • If RR set to low will develop worsening acidosis • Must try to set RR to match their natural compensatory mechanisms How Do We Prevent Electrolyte Catastrophes? • Hourly one touches • Frequent rechecks of lytes and ABG • Utilize the DKA protocol tab on our order set Disposition • In a perfect world all patients go to MICU • In our world – Boarding patients for excessive periods of time – May do a much larger portion of the acute/critical management than in other EDs • How do we know who can go to floor? – – – – – Closure of anion gap Persistent glycemic control K corrected Mental status normal Tolerating PO Pediatric Considerations • Literature suggests 10 cc/kg boluses instead of 20 cc/kg • Cerebral edema is more likely to occur • More likely to have DKA as initial presentation of their diabetes Milwaukee Formula • 1st hour – 10 – 20 cc/kg bolus of NS – Monitor neuro status – Insulin drip 0.05-0.1 U/kg/hr • 2nd hr – resolution – ½ NS (85 ml/kg + maintenance) – initial bolus over next 23 hrs – Continue insulin drip until BS < 250 – Potassium supplementation Moral of the Story • You will see a lot of DKA patients at HF • You may be in charge of their management for a long period of time • You don’t have to rapidly correct the metabolic derangements • Beware of changes in glucose and K levels • Fear cerebral edema • Beware of ventilator induced death Questions/Comments? Thank You!