Pharmacy Consult note: Acute Management of DKA 1000 AM 10/18
advertisement

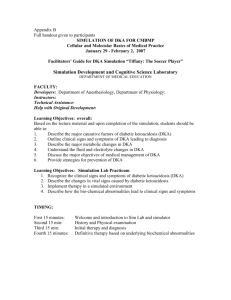
Pharmacy Consult note: Acute Management of DKA 1000 AM 10/18/2013 Patient: Mary McGee S: Patient is 21 yo female with a h/o type 1 DM, diagnosed 3 years ago. Her CC consists of “I felt weak and nauseated during softball practice. I checked my blood glucose and it read ‘HI.’” She complained of fatigue and SOB followed by feeling weak and nauseated. Also very thirsty and seemed “confused”. At that time she checked her meter, and it was disconnected from her pump. She has vomited twice. She’s been using a pump for 6 months now. Her FH is s/o a twin sister with type1 DM. Denies tobacco, alcohol, or illicit drug use. NKDA ROS Complains of blurry vision, lethargy, shortness of breath, nausea, polyuria, and polydipsia. Denies constipation, diarrhea, and headache. O: Medications: NovoLog 100 U/mL, per insulin pump, Glucagon injection kit, as needed Basal rates: 0.8 U/h 1730–0000 0.6 U/h 0000–0300 Correction factor: 1 U:40 mg/dL >120 mg/dL 0.9 U/h 0300–0700 Insulin: carbohydrate ratios: 0.8 U/h 0700–1100 1:10 insulin: carbohydrate before breakfast 0.7 U/h 1100–1730 1:15 insulin: carbohydrate before lunch and dinner PE: Gen: WDWN female, with deep respirations, Lungs: CTA, Kussmaul respirations ketones on her breath, and slurred speech; slightly CV: S1 and S2 normal, RRR; no MRG or S3 or S4 confused, but responds appropriately to questions MS/Ext:No CCE, pulses 2+ throughout, mild calluses VS: BP 101/72, P123, R32, T37.0°C, Wt56, Ht 5'6″ Neuro: A&Ox3; DTRs 2+ throughout; feet w/ HEENT: PERRLA; EOMI; dry mucous membranes normal sensation and vibration Labs: Chem 7:Na 136, K4.8, Cl 101 , CO2 10, BUN 23, SCr 1.4, Glu 479, CrCl 56.2, BMI 19.93 ABG: pH 7.26; pCO2 21 mm Hg; pO2 128 mm Hg; HCO3 7.1 mEq/L; O2 sat 97% UA: + ketones; + glucose ECG: Sinus Tachycardia; Chest X-ray: Normal A: osmolity; 2xNa + (glucose/18) + (BUN/2.8) 2x136 + (479/18) + (23/2.8)=306.81 anion gap: (Na) -(Cl-HCO3) 136-(101+10)= 25 Patient presents with signs and symptoms associated with diabetic ketoacidosis. Insulin insufficiency and possible infection are the risk factors of MM’s DKA. MM is in an acute state and needs to stabilize the serum glucose, electrolytes, and cognitive function. Goals of therapy are to restore perfusion and increase glucose utilization in the periphery, decrease ketogenesis, correct electrolyte imbalances, avoid compilations, and prevent recurrence of DKA. Long term therapeutic goals according to ADA is an A1c% <7, and fasting glucose of 70-130mg/dL. Postprandial glucose should be <180mg/dL. The methodical treatment of DKA includes fluid replacement, correction of hyperglycemia and electrolyte imbalances, and reversal of metabolic acidosis. A subcutaneous insulin regimen should also be reestablished. The ADA recommends initiating an isotonic saline infusion at 15-20ml/kg/hr over the first hour and to monitor cardiac and renal function with a continuous ECG. For MM, this works out to be 1L over the first hour. After that point there is a need to reassess sodium and fluid needs, as well as other electrolyte concerns. At the initiation of fluids, there also needs to be a restart of IV regular insulin at 0.15u/kg bolus and 0.1u/kg/hr infusion. For MM, this works out to be 6 units for both doses. Because insulin causes an intercellular shift of potassium, we will need to supplement the NS solution with 20-30mEq/L at the same rate until MM can handle oral potassium to achieve a concentration of 4-5mEq/L in the blood. After the first hour, if sodium is normal or high, we will need to switch the NS to 1/2NS. In this event, the new rate would be 500ml/hour. We will be checking the blood glucose level every hour. If we do not get a 50mg/dL drop within the first hour, we will double the rate to 12u/h. Our goal is to have a serum blood glucose level <200. When the serum blood glucose level is <200, we can reassess the fluid needs. Change infusion to D5W with ½ saline at a rate of 150-250mL/hr and decrease the insulin infusion to 0.05-0.1 unit/kg/hr. The insulin and dextrose infusion should be adjusted to maintain serum glucose levels between 250-300mg/dl until the plasma osmolality is less than 315mOsm/kg and the patient is mentally alert. According to the ADA, the resolution of DKA is when glucose is less than 200mEq/L, bicarb >18mEq/l, and venous pH is greater than 7.3. Once our patient resolves, we can restart our patient on the pump and educate her on signs and symptoms of DKA as well as informing her to always have a back up if the pump fails. The ADA recommends patients to be started on insulin at the dose they were receiving prior to DKA and further adjusted as needed. Complications of DKA treatment should be monitored for continuously. This includes hypoglycemia, persistent acidosis, hypokalemia, and intracerebral complications. P: 1. Intervention a. 0.9% NS IV infusion at 1L (15 -20ml/kg/h) over the first hour. b. Add 20meQ/L of potassium to infusion c. Recommend IV insulin 6 Unit bolus of regular insulin (0.1 units per kg) followed by 6u/hr 2. After 1 hour a. Reassess urinary output, Chem7, fluid status (BP) b. If sodium is normal or high, start 0.45% NS instead of 0.9% at 500ml/hr c. Check blood glucose, see if it dropped 50 mg/dL i. If not, increase rate to 12u/hr 3. Monitoring a. Monitor blood glucose every hour until less than or equal to 200 mg/dL i. When blood glucose is at 200mg/dL, switch to D5W. b. Monitor electrolytes, BUN, SCr, glucose, osmolality and venous pH every 2-4 hours until stable. c. Monitor vital signs every 30 minutes with continuous ECG d. Monitor with Glascow coma scale every 30 minutes 4. Education a. Signs of DKA (fruity breath, confusion, BG >250mg/dL) and what immediate steps she can take to correct it. Also fatigue and nausea b. Keep Insulin on hand (pens/needles syringe/vials) in case pump fails! Steven Fiedler, Pharm D. Candidate (413)636-2884