Diabetic Ketoacidosis and Hyperglycemia
advertisement

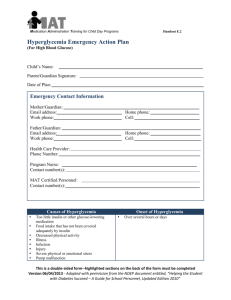
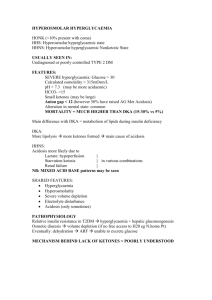
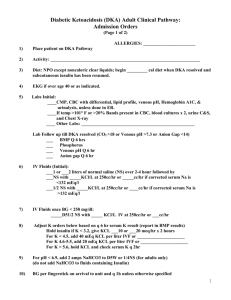
Diabetic Ketoacidosis and Hyperglycemia Valerie Robinson, D.O. Hyperglycemia • • • • Type 1 DM, Type 2 DM, Gestational Diabetes May present with polyuria, polydipsia, weight loss May present with DKA Type 1: usually in children with rapid onset. Caused by autoimmune pancreatic ß-cell destruction, or idiopathic • Type 2: usually in adults with insidious onset. Caused by insulin resistance, insulin secretory defect • Genetic and environmental factors influence development of hyperglycemia. • The main goals of treatment are to alleviate symptoms, minimize the development of long-term complications, enhance the patient's quality of life, and reduce the risk of death. Complications of Hyperglycemia • May lead to DKA, and Hyperosmolar Hyperglycemic State. • Macrovascular disease CAD, MI, CVA, PAD • Diabetic foot ulcers • Microvascular disease nephropathy, retinopathy, neuropathy, Charcot’s foot, ED • Increased risk of infxns and decreased healing • Gestational preeclampsia, SAB, premature labor, polyhydramnios, macrosomia, RDS What is DKA? • Severe electrolyte imbalance with dehydration • Severe insulin shortage • Usually occurs in type 1 but may also occur in type 2 • May be the initial presentation of diabetes mellitus • May be brought on by an infection or another precipitating factor – trauma, CVD, pancreatitis, drugs, ETOH, poor diet Signs and Symptoms • • • • • • • • • Fruity odor to breath (exhaled acetone) Shock Abdominal pain (ileus or delayed emptying) Altered consciousness Nausea/Vomiting Dehydration Polyuria Polydipsia Kussmaul breathing (compensatory hyperventilation) Pathogenesis • Pancreatic islet cells are destroyed, resulting in a lack of insulin and hyperglycemia. • Hyperglycemia induces profound osmotic diuresis, causing water and electrolyte loss, especially potassium. • The body cannot properly use extracellular glucose, so starts producing ketones as an alternate energy source. • Ketosis causes metabolic acidosis. • Metabolic acidosis forces hydrogen ions into cells, displacing potassium ions that are lost through urine and vomiting. Increased anion gap: Usu. >20meq/L Pathogenesis cont. • Total-body potassium depletion is present, but serum potassium levels may be normal or high because of electrolyte shift • Extreme fluid loss results in clinical shock • In some cases, hyperglycemia and dehydration predominate, and acidosis is minimal Tests Results When you suspect DKA, order the following: 1. FSBS/serum glucose 1. >250 mg/dL rarely >800 mg/dL - Used serially to follow tx progress 2. Urine or serum ketones 3. ABG - Used serially to follow tx progress 4. BMP K+ must be monitored closely BUN/Cr used to follow tx progress 5. CBC 6. Blood cultures 2. High levels confirm dx 3. pH <7.3 pCO2 <40 mmHg - confirms dx, reveals severity 4. K+ may be high or normal - K+ may fall rapidly in tx - BUN/Cr reveal dehydration 5. Leukocytosis 6. Possible sepsis Tests cont. Results cont. You may choose to order the following 1. Serum Phosphate, Ca, Mg 1. May be decreased. - May decrease during tx 2. Amylase/lipase 2. May be elevated in DKA - May indicate pancreatitis 3. LFTs 3. Not usually elevated in DKA Do if c/o abdominal pain 4. EKG 4. Look for peaked T or U waves - Look for evidence of precipitating event 5. CXR 6. Lipids 5. Look for precipitating event 6. Likely elevated – aid in ketogenesis Diagnosis • • • • pH <7.3 Hyperglycemia Ketonuria Dehydration • Patient may be asymptomatic, but should still be treated before symptoms occur. Treatment #1: HYDRATION • Hydration with NS. Calculate fluid deficit. Assume 5-10% dehydration if patient is acidotic. • Correct over 36-48 hours. • Usually 500-1000mL bolus in first hour – Children 10-20mL/kg bolus. May use NS, crystalloid, or LR Treatment #2: Insulin • Bolus of 0.1 Units/kg IV • Then 0.1 Units/kg/hour IV – Children: no insulin bolus. 0.05-0.1 Units/kg/hour IV OR (in mild DKA or long transport) Short-acting insulin • Initial dose 0.3 Units/kg SQ • Then 0.1 Units/kg/hour SQ until glucose <250 mg/dL • Then 0.05 Units/kg/hour SQ until DKA is resolved – Children: no insulin bolus. 0.15 Units/kg/2hours SQ or IM Caution: Do not reduce serum glucose by more than 80 mg/dL/hour in children, 80-100 mg/dL/hour in adults Treatment #3: Potassium • 20-40 meq/L added to the IV NS • Titrated to serum K+ concentrations • Usually added after assured of urine output Other Treatment • Bicarbonate may worsen hypokalemia and intracellular acidosis and cause cerebral edema. – Used in ICU when pH <6.9 • Sodium phosphate is not used routinely. – Tx if: <1 mg/dL OR significant cardiac or respiratory compromise. • Dextrose 5% if glucose falls too rapidly and when it falls <250mg/dL. Don’t stop insulin until acidosis is corrected. Caution: If you fail to monitor and replace electrolytes, rehydrate too fast, or reduce glucose too fast, you may cause cerebral edema. – If + cerebral edema, do not replace more than 75% of fluid deficit – May use mannitol 0.5-1.0 g/kg over 20 minutes Follow-up • Look for a cause of the DKA • Make sure glucose is well-controlled at home and patient is educated regarding DKA. Non-Ketotic Hyperosmolar Coma Hyperosmolar Hyperglycemic State • Level of consciousness is depressed when plasma osmolality is high • May be precipitated by concomitant use of certain quinolone antibiotics in patients with diabetes taking certain oral hypoglycemic agents • • • • • • • • Markedly elevated plasma osmolality Severe hyperglycemia >600 mg/dL, may exceed 1000 mg/dL No significant ketonuria/ketonemia No significant acidosis, pH >7.3 and bicarbonate >15meq/L Usually occurs in elderly patients who often have undiagnosed DM2 Thromboembolic complications are common Insulin requirement is less than that for DKA Requires ICU monitoring References • David Toth MD et al. Gestational Diabetes. First Consult . 29 January 2010 • Dennis Saver MD et al. Diabetic Ketoacidosis. First Consult. 27 April 2010. • Abbas E. Kitabchi MD, PhD et al. Clinical features and diagnosis of diabetic ketoacidosis and hyperosmolar hyperglycemic state in adults. UpToDate. 25 June 2012.