Treatment in Cardiac disease - Barwon Division of General Practice
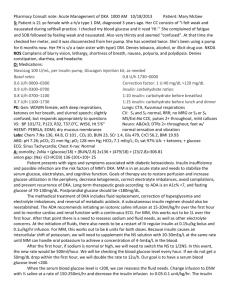
advertisement
Treatment in Cardiac disease The PNs Roll Dr. Sergio Diez Alvarez Staff Specialist Physician Armidale Hospital Main Disorders Hypertension Congestive Cardiac Failure Ischemic Heart Disease Case 1 A 60-year-old woman with a 3-year history of hypertension is seen for worsening dyspnea and cough. She has had chronic obstructive pulmonary disease (COPD) since age 55. She now has dyspnea with walking one-third of a block and a persistent cough. Her hypertension has been managed with diet and exercise. Physical exam reveals an anxious woman with blood pressure 150/86 mmHg, pulse 80, respiratory rate 24, and weight 86 kg. O2 Sat: 88% GP has asked you to discuss some issues with her about her current medical conditions while she waits for her appointment. Issues Salt restriction Exercise Weight loss (BMI & waist circumference) Medication side effects Cardiovascular risk overall – Microalbuminuria, ECG/Echo(LVH) Congestive Cardiac Failure Case 2 A 60-year-old woman with a history of obesity, diabetes, dyslipidemia, and hypertension presented to the GP rooms complaining of fatigue, leg swelling and dyspnoea. She was diagnosed with CCF and started on Lasix 10mg daily at another GP practice. Her diabetes had been managed with metformin alone. Her diet is not good as she eats out a lot, mainly at social gatherings. BP controlled with ramipril. Cholesterol controlled with Lipitor. On examination, blood pressure was 98/64 mmHg, pulse was 92/min, and respirations were 20, weight 98kg. What advice can we give her with regards to her CCF? Issues Salt restriction Fluid restriction “the big Five” – digoxin, frusemide, βblocker, ACEI/ARB, spironolactone Cardiac Rehabilitation CCF is a syndrome - Manage the Aetiology Case 3 A 61-year-old man with prior history of angina complaines of ongoing angina when he walks especially uphill. He is scared of using his anginine “too often as he may get addicted to it”. He has hypertension and dyslipidaemia. He had a stent put in 3 years ago for “a blockage” Smokes only when goes to the pub Tries to exercise but worried about the chest pain medications included: Diltiazem CD 180 mg daily Aspirin 100mg Anginine spray prn He is supposed to be on Simvastatin but it gives him sore muscles so he only takes it on the days he gets chest pain BP 140/90mmHg, HR 78/min, weight 102kg Laboratory investigations: Glucose 8.1mmol/l, cholesterol 4.6mmol/l What advice can you give him? Issues Angina management in general Advice on lifestyle modifications Assess precipitants of angina Assess need for further investigations She was re-admitted with hyperglycemia as she had run out of insulin During the 3-day hospital stay, she required 2 IU of regular IV insulin per hour to maintain blood glucose levels in the range of 9-11mol/l. She was sent home on NPH insulin 25 IU twice daily and metformin 500 mg also twice daily. Pioglitazone was discontinued because of the history of liver disease. She returned 10 days after discharge with nausea, vomiting, polyuria, polydipsia, and general malaise Diabetic ketoacidosis (DKA) was diagnosed and the patient was started on an insulin drip. Two days later the drip was discontinued and she was started on Novomix 30 twice daily and regular coverage. Despite increasing the daily doses of insulin to 112 IU daily, her glucose continued to increase into the range of 1215mmol/l and the acidosis worsened. She was found to be suffering from DKA again with a bicarbonate level of 12 mEq/dL and positive ketones in blood. An insulin drip was started again and she was transferred to the ICU. Over the next several days, the drip was increased up to 12 IU per hour . Blood glucose levels decreased slowly into the 9mmol/l range and bicarbonate normalized. After extensive discussions, it was decided to start metformin 500mg bd despite the past history of autoimmune liver disease. The blood glucose continued to decrease and finally stabilized in the range of 8-10mmol/l. The patient was transferred to the regular floor after a total of 9 days in the ICU. She is due for discharge, what regimen do you use?