Mel`s Mechanical Ventilation Outline
advertisement
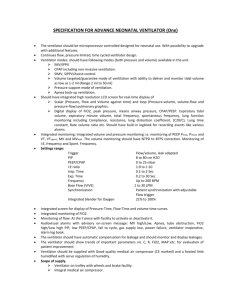
Mechanical Ventilation Lecture Outline Pulmonary Terminology. Mechanical Ventilation: Indications. Types. Mechanics. Modes of Mechanical Ventilation. Mechanical Ventilator Alarms. Weaning. Reading Assignment Brunner 11th ed., chapter 25 Mechanical Ventilation: Indications. Classification of ventilators. Complications with mechanical ventilation. Weaning parameters. Pulmonary Terminology Respiratory Rate (f) Breaths per minute. Patient Normal: 12 – 20 breaths/minute. Rates > 30: Rates > 40: Ventilator Normal: 8 – 12 breaths/minute. Ventilator can provide ALL of patient’s breaths, OR the patient may be able to breathe spontaneously between ventilator breaths. Tidal Volume (Vt) Volume in one breath. POSITIVE PRESSURE Volume of gas delivered with each ventilation. Normal is 5 – 8 cc/kg (ideal body weight). **too much can cause volutrauma. It will often be set a higher rate lower volume Minute Volume / Minute Ventilation (VE) Volume of air that is moved through the lungs over 1 minute. **This regulates CO2 and acid/base Vt x Rate (ventilator / patient). Normal: 5 – 10 liters. (Never < 5L) Increased VE: Hyperventilation. Decreased VE: Hypoventilation. Example: Vt x Rate (ventilator / patient). 0.4 L x 8 breaths = 3.2 L/min. 0.7 L x 12 breaths = 8.4 L/min. 0.8 L x 24 breaths = 19.2 L/min. – look at ABG you will see alkalosis Vital Capacity (VC) Maximum amount of air exhaled after a maximum inspiration. Normal 65 cc/kg (IBW). before extubation. Diaphragm function. Fraction of Inspired Oxygen (FiO2) Amount of oxygen being delivered (%). Usually the FiO2 will be adjusted to keep the SaO2 > 90% OR PaO2 > 60 mm Hg. Remember oxygen toxicity! Occurs with FiO2 > 50% – 60% for > 24 hours. Negative Inspiratory Force (NIF) Negative Inspiratory Pressure (NIP) How much negative pressure change can the patient generate with maximum inspiratory effort. Normal range: -80 cm to -100 cm H2O. before extubation. Need at least -20 cm to maintain minute ventilation (VE). Peak Inspiratory Pressure (PIP) How much pressure is reached in the lung at the peak of inspiration (after giving set Vt). Do not want high pressures. Volutrauma in 50+ pressures. Stiff lungs = High pressure. Very important parameter to measure – because of compliance – if compliance is down pressure increases-this will put a pt a great risk for pneumothorax PEEP Positive End Expiratory Pressure Low PEEP = 1 – 5 cm H2O. Moderate PEEP = 5 – 15 cm H2O. High PEEP = > 15 cm H2O. Optimum PEEP = Helps with oxygenation Keeps alveoli open Minimizes shunting Caution at high levels AUTOPEEP – a nautrual change in PEEP setting due to the fact that pt is not exhaling as much as they were before (AIRTRAPPING) PIP & PEEP High levels - increase volutrauma - increase chances for pneumothorax - decrease venous return to heart - may cause hypotension - increase auto PEEP Sensitivity Sensitivity function controls the amount of patient effort needed to initiate an inspiration. Measured by negative inspiratory effort. Usually set at minus (–) 2. Indications-Types-Mechanics Indications Supporting gas exchange. lung volume. work of breathing. Reverse hypoxemia & resp. acidosis. Relieve resp. distress. Preventing resp. muscle fatigue. Permit sedation & neuromuscular blockade. Stabilize chest wall. Decrease oxygen consumption. Types of Ventilators Negative Pressure Ventilators: Applied externally to the patient. Example: Ventilator or iron lung. Positive Pressure Ventilators: Forces air into the lungs via endotracheal tube or tracheostomy. Iron Lung – Polio Patient Ventilator Mechanics Trigger. Event that begins inspiration. Patient-initiated respiratory effort. Machine-initiated positive pressure. Limit Limits / maintains airflow during inspiration. Flow-Rate (IFR). How fast is air pumped into lungs? Set Pressure (Pressure Control) (PIP). How much pressure is reached at peak of inspiration? Volume-limited (Volume control) (VT). How much volume of air is given with each breath? Cycle. Event that ends inspiration. Volume cycled ventilation. Pressure cycled ventilation. Pressure support ventilation. Modes of Mechanical Ventilation Assist Control (AC). Initial mode of choice! Synchronized Intermitted Mandatory Ventilation (SIMV). Pressure Support Ventilation (PSV). Continuous Positive Airway Pressure (CPAP). Bilevel Positive Airway Pressure (BIPAP). Assist Control (AC) Set Vt, RR, FiO2, &/or PEEP. Trigger that initiates inspiration can be either ventilator or pt’s respiratory effort. If pt initiates breathes faster- receives set Vt, FiO2 & PEEP from the ventilator. If pt breathes slower ventilator delivers set Vt, at set rate, FiO2 & PEEP. ALL breaths are delivered by ventilator at set Vt, FiO2 & PEEP. Synchronized Intermittent Mandatory Ventilation (SIMV) Vt, rate, FiO2, PEEP, & sensitivity are preset. All breaths taken above the set rate are spontaneous breaths. ** Trigger may be spontaneous or mandatory the ventilator delivers breaths at set Vt, rate, FiO2 &/or PEEP. Synchronized Intermittent Mandatory Ventilation (SIMV) All breaths are synchronized. Mandatory breaths – set tidal volume Spontaneous breaths – patient tidal volume SIMV Advantages: Strengthens respiratory muscles. PSV can be added. Lower mean airway pressure. Disadvantages: Increased WOB. Not tolerated well by some patients. Pressure Support Ventilation (PSV) No set Vt or rate. (this is a weaning mode) Patient’s effort determines RR, IFR, Vt. Delivers air to a set pressure early in inspiration. Pressure is maintained throughout inspiration. PSV Advantages: Increased patient comfort. Decreased muscle fatigue. Respiratory conditioning. Can be added to SIMV to enhance weaning. Decreased WOB/O2 consumption. Disadvantages: DO NOT over sedate. Monitor closely. Can be difficult for patient. Continuous Positive Airway Pressure (CPAP) Spontaneous breathing mode. Positive pressure that is maintained throughout respiratory cycle. Usually 5 to 10 cm H2O pressure. Patient generates own rate & tidal volume. Similar to PEEP. Used for intubated & non-intubated patients. Used as weaning mode. Used for nocturnal ventilation. Same as SIMV with PEEP. Often used for obstructive sleep apnea. CPAP Mode BiPAP Noninvasive, noncontinuous, Bilevel Positive Airway Pressure. Provides both inspiratory & expiratory pressure support. Weaning. Hypoventilation. Sleep apnea. Mechanical Ventilator Alarms & Humidification Ventilator Alarms Low pressure alarms. (tube disconnected may be a common cause) High pressure alarms. (coughing, tube kinked) Peak Inspiratory pressure (PIP) Apnea alarm: ALWAYS have AMBU bag at bedside. Pressure Alarms Peak Inspiratory Pressure: Decreased compliance. Kinked ET tube Mucous plug. Increased secretions. Water in circuit. pneumothorax MONITOR trends. Low pressure alarms: Cuff leak. Dislodged ET tube Broken circuit. Troubleshooting? Remember DOPE Dislodged Obstructed Pneumothorax Equipment failure Always check the patient, not the monitor!!! Patient-Ventilator Dysynchrony Patient appears to be fighting or “bucking” the ventilator. Decreases effectiveness of mechanical ventilation, development of auto-PEEP, psychological distress. Adjust ventilator settings to accommodate patient’s spontaneous breathing pattern. Sedation or neuromuscular blockade. E.g., Diprivan drip. Humidification Why should we humidify & warm air delivered by artificial airways? What would happen if there was no humidification? 100% humidity at 37 oC. Prevent water condensation build up – tubing needs to be drained. Ventilator Complications Aspiration: Before, during & after intubation. ARDS & Pneumonia (VAP): Risk Factors: Brushing Teeth: Ventilator Patient Volutrauma (Barotrauma): Mechanical ventilation & PEEP can over distend & rupture alveoli air leakage. GI Complications: Distention. Ileus (Gastroparesis). Stress ulcers. Cardiac Complications: Mechanical ventilation & increased PEEP increased intrathoracic pressure decreased venous return to right heart decreased preload decreased CO decreased hepatic, renal, CNS (increased ICP) perfusion. Anxiety: Dependent on machine to breathe & unable to speak. Nutritional Support Why should we feed our ventilated patients? Respiratory muscles need energy to work muscle fatigue & decreased tidal volume. Body cannibalizes intercostal & diaphragmatic muscles for energy. Long-term mechanical ventilation patients need 2000 - 2500 kcal/day. Begin by 3rd day of intubation. Malnourished – within 24 hours of intubation. Enteral route vs. TPN. Prerequisite for weaning! Weaning Gradual withdrawal of mechanical ventilation & reestablishment of spontaneous breathing. Begin only after cause for respiratory failure is corrected & patient is stable. Factors to Consider: Length of time on ventilator. Sleep deprivation. Nutritional status. No sepsis. Adequate respiratory muscle function. Readiness to Wean LOC, spontaneous breathing, respiratory rate & pattern. Physiologic & hemodynamic stability. Adequacy of oxygenation & ventilation. Rested with no suppressant drugs. Breathing Trials: Ø accessory muscle use, retractions, or paradoxical breathing. ABG: Ø rising CO2 or falling pH. Secretions? Cough? Weaning Criteria PaO2: > 60 – 80 mmHg. FiO2: 50%. PEEP: 5 cm H2O. SaO2: > 90%. PaO2:FiO2 ratio: > 150 or 200. Vital Capacity: 10 to 15 ml/kg or > 800 cc. Negative Inspiratory Pressure (Force) (NIP or NIF): Minus (-)30 cm H2O or less. Respiratory Rate (f): > 12 & < 30 Tidal Volume: > 5 cc/kg. Example: Pt weighs 80 kg. 80 X 5 = 400 cc. Minute Ventilation: 5 – 10 L/minute. Examples: RR 30. VT 900 cc RR 8. VT 300 cc Ratio of Resp. Rate : Tidal Volume (liters) = Rapid Shallow Breathing Index (RSBI) < 100* is predictive of weaning success. RSBI = f / Vt Examples: f = 40; Vt = 300. f = 20; Vt = 400. f = 18; Vt = 600. f = 35; Vt = 250. Weaning Methods: SIMV Place ventilator in SIMV mode & slowly decrease rate until zero (4). Obtain ABG 30 minutes afterwards. Can increase work of breathing. Monitor for signs of respiratory muscle fatigue PSV. Benefit: Ventilator backup if patient fails to breath. Alarms will sound. Weaning Methods: T-Piece Remove patient from the ventilator & have patient breath spontaneously on a T-piece. Monitor patient's response & tolerance. Duration of T-piece is dependent on MD. After a set amount of time, the patient is placed back on ventilator (trials of increasing frequency & duration). May add CPAP. Weaning Methods: PSV Augments patient’s spontaneous breathing with positive pressure “boost” during inspiration. Gradually decrease level of PSV while maintaining spontaneous tidal vol. (Vt) of 8 – 12 ml/kg & RR < 25 breaths/minute. If the patient is able to maintain adequate spontaneous breathing at this level – extubation is considered. Example: COPD Exacerbation 8/22/05: On Vent. Time: 0659 FiO2: 40%. VT: 700. SIMV: 4. PEEP: 3. pH: 7.36 PCO2: 52.1 HCO3: 28.6 PO2: 81.1 Interpretation: Respiratory acidosis. Full compensation. 8/23/05: T-Piece Trial Time: 0556 FiO2: 40% pH: 7.28 PCO2: 66.2 HCO3: 30.4 PO2: 107 SaO2: 97% Interpretation: Respiratory acidosis. Partial compensation. Would you wean this patient at this time? 8/23/05: CPAP Time: 0816 FiO2: 40% pH: 7.32 PCO2: 54.7 HCO3: 33.3 PO2: 74.8 SaO2: 94.8% Interpretation: Respiratory acidosis. Partial compensation. Would you wean this patient at this time? 8/24/05: T-Piece Trial Time: 0658 FiO2: 35% pH: 7.35 PCO2: 47.9 HCO3: 29.8 PO2: 126 Interpretation: Respiratory acidosis. Full compensation. Would you wean this patient at this time? Patient weaned off ventilator & extubated. 2L NC.