Initiation and weaning of mechanical ventilation
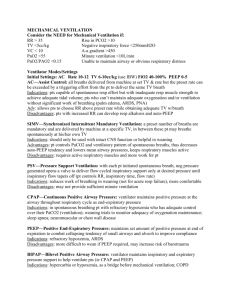
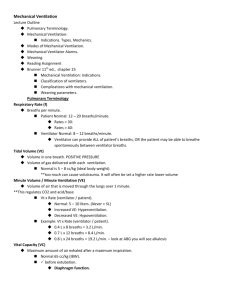
advertisement

INITIATION AND WEANING OF MECHANICAL VENTILATION BY AHMED MOHAMED HASSAN OUTLINE Definition. Indications Ventilator Settings Modes of Ventilation Weaning Summary DEFINITION Use of a mechanical apparatus to provide the requirements of a patient’s breathing. Use of positive pressure to physically transport gases into and out of lungs (earlier ventilators used negative pressure) Usually performed via ETT but not always (noninvasive ventilation) MECHANICAL VENTILATION ( MV ) A supportive measure – not a therapy Must diagnose and treat underlying cause Used to support &/or rest patient until underlying disorder improved INDICATIONS FOR MV Acute resp failure: ARDS Heart failure. Pneumonia Sepsis. Complication of surgery. Trauma Acute exacerbations COPD. Neuromuscular diseases. VENTILATOR SETTINGS FIO2 Volume (VT) Rate Pressure PEEP I:E Flow rate VENTILATOR SETTINGS Fraction of inspired oxygen (FiO2): Target Sao2 90 % & Pao2< 60mmHg. Atempt to keep FiO2 <50% to avoid O2 toxicty. Tidal volume (Vt): Is constant in volume-cycled modes and variable with in pressure-limited modes. In patients without lung disease Vt of 8 - 10 mL/kg . Lower Vt 6 ml/kg are recommended for ARDS, & Vt 8 mL/kg is recommended in patients with asthma, COPD(as long as no increase in plateau presure). VENTILATOR SETTINGS Respiratory rate (RR): 12 and 20 breaths per minute is reasonable. Determine minute ventilation. Minute ventilation (VE): Is the product of the Vt and RR. V is based on PaCO2 as a marker of ventilatory requirements. V of approximately 5 L/min maintain normocapnea. Permissive hypercapnia is allowed in ARDS and status asthmaticus. E E VENTILATOR SETTINGS Inflation pressure limit: High inflation pressures cause barotruama. Increased Pplat, is most injurious, reflecting alveolar overdistention and not airway resistance. Pplat > 30 cm H2O is recommended. Inspiratory Sensitivity : It is the drop in airway pressure that is required before the ventilator senses the patient's effort. 0.5 to 1 cm H2O allow very weak patients to initiate a breath, Higher values make triggering more difficult. VENTILATOR SETTINGS Inspiratory flow rate: The ratio of Vt to inspiratory flow rate determines inspiratory time (Ti). inspir flow rate Ti time for expiration auto PEEP. inspir flow rate PIP & not Pplat. COPD & asthma the expiratory time should be increased to allow exhalation of trapped gas. Positive end-expiratory pressure (PEEP): PEEP is the maintenance of positive pressure after expiratory flow is completed. Useful to treat refractory hypoxemia Complication: Hypotension Diastolic dysfunctions Barotrauma MODES OF MV MV may be: Invasive, delivered through an endotracheal tube (ETT) or tracheostomy tube. Noninvasive positive pressure ventilation (NIPPV) interfaces the ventilator with the patient through a full-face or nasal mask. MOODS OF MECHANICAL VENTILATION Volume cycled MV: Pressure-limited MV: Delivers a preset (Vt) specified by the operator. Delivers a flow until a preset pressure limit that is set by the operator is reached. (PIP) are, depending on the patient's compliance. PIP is always the same but Vt is variable, according to the patient's compliance. Examples: • Pressure Support Ventilation (PSV) • Pressure Control Ventilation (PCV) • CPAP • BiPAP Examples: • Assist/Control • Intermittent Mandatory Ventilation (IMV) • Synchronous Intermittent Mandatory Ventilation (SIMV) PRESSURE SUPPORT VENTILATION(PSV) Every breath is an assisted breath. The patient determines the inspiratory flow rate and the RR. Advantages: Better patient synchrony Limits Peak inspiratory Pressure. Disadvantages: Inadequate volumes if the ETT is blocked or decreased lung compliance. Apnea backup is less supportive than that of AC PRESSURE CONTROL VENTILATION (PCV) Controlled breaths are delivered at a preset time interval. RR, maximal pressure limit are both controlled. Spontaneous breaths is allowed between the mandatory breaths. Advantades: Decrease risk of barotrauma Used in inverse ratio ventilation. Disadvantages: Cannot ensure minimal VE CONTINUOUS POSITIVE AIRWAY PRESSURE (CPAP): Used for oxygenation and as a mode of weaning. patient assumes most of the work of breathing & determine RR, Vt & VE. BIPAP Ventilator delivers two levels of positive airway pressure for preset periods of time. Advantages: Decreased requirement for sedation. Used in Obstructive Sleep Apnea. Disadvantages: Theoretical risk of over-distension of lungs. ASSIST CONTROL (AC): Pt RR < preset rate so all breath will be assisted. Pt RR > preset rate so all breath will be controlled. Advantages: Ensures a minimum VE. Better patient synchrony. Disadvantages: Induce respiratory alkalosis if high respiratory drive (i.e., liver failure). INTERMITENT MANDATORY VENTILATION (IMV) Ventilator will deliver a preset volume at a specific time intervals. Different from Controlled mode: pt can initiate spontaneous breaths. Different from Assisted mode: spontaneous breaths are not supported by machine. Advantages: Assures a VE Disadvantages: Patient asynchrony. SYNCHRONIZED INTERMITTENT MANDATORY VENTILATION (SIMV): Delivered spontaneous, assisted, and mandatory breath. Most commonly used mode. Advantages: Ensures a minimum VE. Disadvantages: The worst mode of weaning. NONINVASIVE VENTILATION Avoids intubation and complications. Can deliver various modes of ventilation Indications: Hypercapneic respiratory failure (COPD exac). Cardiogenic pulmonary edema. Hypoxic respiratory failure. Contraindications: Inability to cooperate (i.e. Confusion). Inability to clear secretions. Hemodynamic instability. Frature skull base as it may cause pneumoencephaly. NEW MODES OF MV Volume Support. Pressure-Regulated Volume Control (PRVC). Volume-Assured Pressure Support. Automode. Adaptive support ventilation (ASV). Proportional Assist Ventilation(PAV). Mandatory Minute Ventilation. Airway Pressure Release Ventilation (APRV). WEANING When: The underlying pathology improves. Hemodynamically stable. Oxygenation: PaO2/FiO2 >200, PEEP<7.5 cm H2O, FiO2<0.5 Indices: Rapid shallow breathing: RR/Vt > 105 positive predictive value of 78%. RR/Vt < 105 negative predictive value of 95 %. Maximal Inspiratory Pressure(Pmax) Excellent negative predictive value if less than –20 cm H2O . WEANING Methods: Spontaneous breathing trials: complete withdrawal of MV Only one trial every 24-hour CPAP: Allow monitoring of RR, Vt & VE Pressure support ventilation (PSV) SIMV: Gradual reduction in the level of PSV The worst mode of weaning. Duration: Short-term MV (<21 days) prolonged MV (>21 days) 30 to 120 minutes at least 24 hours. CAUSES OF WEANING FAILURE Auto-PEEP. Poor nutritional status. Overfeeding. Left heart failure. Decreased magnesium and phosphate levels. Infection/fever. Major organ failure. SIGNS OF WEANING FAILURE Clinical criteria : Diaphoresis . Increased respiratory effort . Paradoxical breathing & use of accessory respiratory. Cardiac: HR < 30 beats/min over baseline. Profound bradycardia. Ventricular ectopy. Supraventricular tachyarrhythmias. Mean arterial blood pressure equal to or greater than 15 mm Hg or equal to or less than 30 mm Hg from baseline. SIGNS OF WEANING FAILURE Respiratory: RR < 35 breaths/min . SaO2> 90%. PaCO2 50 mmHg or increase >8 mmHg. pH<7.33 or decrease >0.07. PaO2 60 mm Hg with FiO2 of 0.5. Ventilator management algorithim Modified from Sena et al, ACS Surgery: Principles and Practice (2005). Initial intubation • FiO2 = 50% • RR = 12 – 15 • PEEP = 5 • VT = 8 – 10 ml/kg SaO2 < 90% SaO2 < 90% • • • • Increase FiO2 (keep SaO2>90%) Increase PEEP to max 20 Identify possible acute lung injury Identify respiratory failure causes No injury Acute lung injury • Low TV (lung-protective) settings • Reduce TV to 6 ml/kg • Increase RR up to 35 to keep pH > 7.2, PaCO2 < 50 • Adjust PEEP to keep FiO2 < 60% SaO2 < 90% • Associated conditions (PTX, hemothorax, hydrothorax) • Consider adjunct measures (prone positioning, HFOV, IRV) SaO2 > 90% • • • • Adjust RR to maintain PaCO2 = 40 Reduce FiO2 < 50% as tolerated Reduce PEEP < 8 as tolerated Assess criteria for SBT daily Fail SBT Acute lung injury SaO2 < 90% SaO2 > 90% SaO2 > 90% SaO2 > 90% • Continue lung-protective ventilation until: • PaO2/FiO2 > 300 • Criteria met for SBT Persistently fail SBT • Consider tracheostomy • Resume daily SBTs with CPAP or tracheostomy collar Pass SBT Airway stable Airway stable Pass SBT Intubated > 2 wks Prolonged ventilator dependence • Consider PSV wean (gradual reduction of pressure support) • Consider gradual increases in SBT duration until endurance improves Pass SBT Extubate SUMMARY Mechanical ventilation used to: 1. 2. 3. 4. 5. Improve oxygenation. Improve ventilation (CO2 removal). Unload respiratory muscles. Neuromuscular diseases. Decrease intracranial tension. A support until patients condition improves SUMMARY Different modes for ventilation Differ in how breaths are initiated, ended and assisted. No proven advantage of one mode over the other. Use ventilator strategies to avoid volutrauma and other adverse effects. Numerous trials performed to develop criteria for success weaning, however, not very useful to predict when to begin the weaning and physicians should rely on clinical judgement also. SUMMARY Daily screening may reduce the duration of MV and ICU cost. The removal of the artificial airway from a patient who has successfully been discontinued from ventilatory support should be based on assessment of airway patency and the ability of the patient to protect the airway. Patients receiving MV who fail an SBT should have the cause determined. SUMMARY Tracheostomy should be considered after it becomes apparent that the patient will require prolonged MV. Thank you