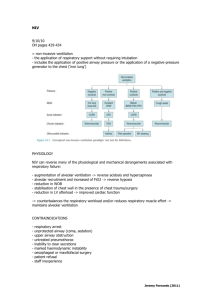
Non-invasive Ventilation
advertisement

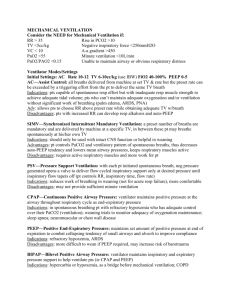
Non-invasive Ventilation Dr Liam Doherty, Consultant Respiratory Physician, Bon Secours, Cork Positive Airway Pressure CPAP = continuous positive airway pressure BiPAP = Bilevel positive airway pressure = Inspiratory pressure (IPAP) and expiratory pressure (EPAP) Why? Invasive ventilation Sedated Can’t speak Can’t eat High infection risk Increased bleeding risk Barotrauma Limited ICU beds Non-invasive ventilation Not sedated Can speak Can eat Low infection risk Available on wellsupervised medical wards How does it work? In summary Stents airway Recruitment of alveoli Decreases right to left intrapulmonary shunting Decreases work of breathing Overcomes PEEPi Lowers left ventricular transmural pressure reducing afterload and increasing cardiac output Who gets NIV? Acute Type 2 Respiratory failure COPD, pH <7.35 despite maximum Rx on controlled O2 Cardiogenic pulmonary oedema with hypoxia. Decompensated obstructive sleep apnoea. Chest wall trauma who remain hypoxic. (CPAP) Diffuse pneumonia who remain hypoxic despite maximum Rx (CPAP) Weaning from invasive ventilation. Who can’t have NIV? Recent facial or upper airway/upper GI surgery, Facial burns or trauma, Fixed obstruction of the upper airway, Vomiting. Inability to protect the airway, Copious respiratory secretions Life threatening hypoxaemia, Severe co-morbidity, Confusion/agitation, Bowel obstruction. Which ventilator Types of NIV Negative pressure ventilation e.g. “iron-lung”, tank, shell, cuirass, rocking bed, pneumo-belt Positive pressure ventilation Pressure limited (CPAP, Bilevel PAP) Volume limited N.B. Diaphragm-pacing, glosso-pharyngeal breathing, cough insufflator-exsufflator Which interface How do you commence NIV? Monitoring progress Oximetry Respiratory rate Patient comfort PCO2 Patient-ventilator synchronisation Give breaks for drinks/food Keep on for as long as possible (2 days+) When things go wrong! Is ventilation inadequate? Observe chest expansion Increase target pressure (or IPAP) or volume Consider increasing inspiratory time Consider increasing respiratory rate (to increase minute ventilation) Consider a different mode of ventilation/ventilator, if available Is the patient synchronising with the ventilator? Observe patient Adjust rate and/or IE ratio (with assist/control) Check inspiratory trigger (if adjustable) Check expiratory trigger (if adjustable) Consider increasing EPAP (with bi-level pressure support in COPD) Downside to NIV Horrendous to wear Can’t talk Can’t eat/drink Can’t sleep Agitation, claustrophobia Poor synchrony Delays intubation Final messages Give appropriate oxygen! Non-invasive ventilators just blow air Try to synchronise ventilator to patient i.e. ventilator should support normal ventilation When in doubt use CPAP NIV doesn’t work for everyone (30% failure rate) Never forget need for intubation!