CONTROL OF CARDIAC OUTPUT - UCLA Department of Surgery
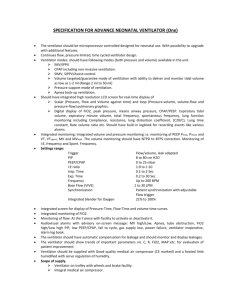
advertisement

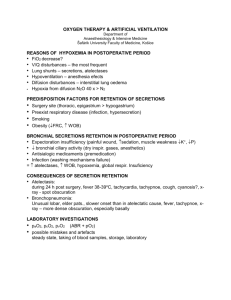
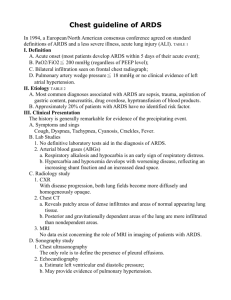
Introduction to Critical Care Daniel R. Margulies, MD, FACS Director, Trauma and Surgical Critical Care Department of Surgery, CSMC C S Los Angeles, California Introduction to Critical Care What’s so Special about the ICU? Ventilators Hemodynamic Monitoring Vasoactive Drugs “Applied Physiology” Introduction to Critical Care Basic Ventilator Management Indications for Ventilation Inability to Ventilate (high pCO2) COPD Inability to Oxygenate (low pO2) ARDS Mixed common Introduction to Critical Care Intubation Orotracheal Nasotracheal Cricothyrotomy Tracheostomy Introduction to Critical Care Ventilator Orders Initial Ventilator Orders : Volume cycled FiO2 Rate Mode (AC, SIMV, PC, PS, CPAP) PEEP TV Consider NG tube, art line, restraints Check the CXR!! Introduction to Critical Care Ventilator Changes pO2: keep FiO2 <60% PEEP FiO2 pCO2 TV Rate Ventilator Changes Introduction to Critical Care pO2 = 380 FiO2=100% What now? Ventilator Changes Introduction to Critical Care Remember the “Rule of 7s” Each % change of FiO2 of 1 results in a change of pO2 of 7 pO2 - 100 FiO2 = ------------------7 Introduction to Critical Care Weaning PaO2 >60 on FiO2 < 0.5 with PEEP <5 Minute vent <10 L/min NIF more negative than -20 VC >800 mL TV >300 mL Use T-piece or CPAP with PS Introduction to Critical Care After Extubation Oxygen Mask Check ABG Cough / Deep Breathing Incentive Spirometer Introduction to Critical Care ARDS 1. Impaired Oxygenation: PaO2/FiO2 ratio < 200 (normal > 450) 2. Bilateral pulmonary infiltrates on CXR 3. PCW < 18 (no CHF) ARDS is an acute clinical illness characterized by severe hypoxemia and bilateral infiltrates on chest X-ray in the absence of pulmonary edema. Introduction to Critical Care Causes • Infection sepsis • Trauma hemorrhagic shock • Multiple transfusions • Low flow state from any cause • Aspiration pneumonia • Acute pancreatitis • Smoke inhalation • and many more….. Introduction to Critical Care Levy G, Shabot MM, Hart M, et al: Transfusion associated noncardiogenic pulmonary edema. Transfusion 1986;26: 278. Introduction to Critical Care Pathophysiology • Large alveolar surface area = 70 m2 (skin = 1.7 m2) • Lung sensitive to noxious stimuli - inhaled and circulating • Lung receives entire cardiac output every minute • Affected by multiple inflammatory mediators and cells Introduction to Critical Care Cells Inflammatory Mediators • • • • • • • • • • Thromboxane A2 Prostacyclin Leukotrienes Platelet-activating factor (PAF) Bradykinin C3a, C5a Tumor necrosis factor IL-1, IL-6 Elastase, Collagenase Oxygen free radicals • • • • • • • • Leucocytes Macrophages Monocytes Endothelial cells Mast cells Bosophils Fibroblasts Platelets Nothing New…... Still can’t do anything about ‘em! Introduction to Critical Care Causes & Time of Death After Multiple Trauma Introduction to Critical Care New Ventilator Strategies - I Goal: Reduce Alveolar distention Marcy & Marini. Chest 1991;100:494 Introduction to Critical Care New Ventilator Strategies • Permissive hypercapnia • Pressure controlled ventilation • Pressure release ventilation • Low volume pressure-limited ventilation • Inverse ratio ventilation • Prone ventilation Introduction to Critical Care Permissive Hypercapnia Tolerate mild to moderate respiratory acidosis (elevated PCO2) in order to reduce airway pressures. • Lower tidal volumes • Lower respiratory rates • Lower peak and mean airway pressures Introduction to Critical Care Prone Positioning Stocker et al. Chest 1997;111:1008 Introduction to Critical Care Extracorporeal CO2 Removal (ECCO2R) Status: Ineffective Guinard et al. Clin Invest Crit Care 1997;111:1000 Introduction to Critical Care Other New Ventilator Strategies • High frequency ventilation (>60/min) • High Positive End-Expiratory Pressure (PEEP) ventilation • Extra-corporeal membrane oxygenation (ECMO) • Extra-Corporeal CO2 Removal (ECCOR) • Partial Liquid Ventilation ? Introduction to Critical Care Partial Liquid Ventilation Leach et al. Crit Care Med 1993;21:1270. Introduction to Critical Care Partial Liquid Ventilation PaO2 PaCO2 Status: Unproven pH Conventional Vent Partial Liquid Vent Introduction to Critical Care New Pharmacologic Strategies • Inhaled nitric oxide (NO) • Surfactant replacement • Ketoconazole • Prostaglandin E1 • Non-steroidal anti-inflammatory agents • High dose steroids (again) Introduction to Critical Care Pharmacologic Treatment of ARDS Kollef & Schuster. NEJM 1995;332:27. Introduction to Critical Care How the SICU Does It Patient R.N. • 31 y/o female • 2 days S/P laparoscopic GYN procedure • Found hypotensive, febrile on ward • CT abdomen - fluid collections & air • OR SB perf + massive contamination • SICU postop - hypotensive on vent Introduction to Critical Care 4/5 Introduction to Critical Care 4/11 Introduction to Critical Care Surgical ICU Management • Hemodynamic/Swan-Ganz monitoring • Volume resuscitation > 20L (sepsis) • Triple antibiotics • Dopamine, neosynepherine • CT guided abscess drainage • Repeat laparotomy & drainage Introduction to Critical Care 4/13/ Introduction to Critical Care Ventilator Management • A/C volume vent Pressure Control vent • Inverse Ratio ventilation • Paralysis & sedation > 10 days • Permissive hypercapnia • High PEEP (as required) 15 cm H2O • High FiO2 (as required) 100% ~ 7 days • Tracheostomy Introduction to Critical Care 4/20 Introduction to Critical Care ARDS Management Principles ? Brandstetter RD. Heart Lung 1997;26: 3-14 Introduction to Critical Care ARDS Prognosis - Overall Milberg at al. JAMA 1995;273:306. Introduction to Critical Care The News on ARDS in Summary The good news is……. The prognosis and survival for ARDS is improving! The bad news is……. WE’RE NOT EXACTLY SURE WHY! Introduction to Critical Care Hemodynamic Monitoring and Vasoactive Drugs SHOCK Introduction to Critical Care A state in which tissue perfusion and/or nutrient uptake fails to meet the body's metabolic needs. Shock can occur with low, high or normal cardiac output. Cardiogenic Hypovolemic Septic Neurogenic Cardiac compressive CONTROL OF CARDIAC OUTPUT Introduction to Critical Care PRELOAD left ventricular end diastolic pressure AFTERLOAD pressure against which the left ventricle must eject blood HEART RATE CONTRACTILITY strength of left ventricular contraction CONTROL OF CARDIAC OUTPUT Introduction to Critical Care Pulmonary Artery Catheter Introduction to Critical Care Starling Curves Introduction to Critical Care Catheter Insertion Waveforms Introduction to Critical Care CONTROL OF CARDIAC OUTPUT Introduction to Critical Care CONTROL OF CARDIAC OUTPUT Introduction to Critical Care • Normal Hemodynamic Parameters : • MAP - 70-110 mmHg • SVR - 900-1200 dynes/cm square • PVR - 80-120 dynes/cm square • CO - 4-7 L/min CONTROL OF CARDIAC OUTPUT Introduction to Critical Care • Normal Hemodynamic Parameters : • DO2 - 700-1400 ml/O2/square meter • VO2 - 180-280 ml/O2/square meter • O2 extraction - 20-30% • Qs/Qt - 3-5% • Ca O2 - 16-22 vol% • Cv O2 - 12-16 vol% Hemodynamic Parameters Introduction to Critical Care SVR = ( MAP - RAp/ CO ) x 80 - systemic vascular resistance PVR = ( PAP - PAOP/ CO ) x 80 - pulmonary vascular resistance CO = VO2 / ( CaO2 - CvO2 ) - cardiac output DO2 = CO x Ca O2 x 10 - Oxygen delivery MAP = mean arterial pressure, PAP = pulmonary artery pressure, RAp = central venous pressure ( RA pressure ), PAOP = pulmonary artery occlusion pressure ) Hemodynamic Parameters Introduction to Critical Care VO2 = ( Ca O2 - Cv O2 ) x CO x10 - Oxygen consumption Ca O2 = ( 1.39 x Hb x SaO2 ) + ( 0.003 x PaO2 ) - Arterial O2 content Cv O2 = ( 1.39 x Hb x SvO2 ) + ( 0.003 x PvO2 ) - Venous O2 content •O2 extraction = VO2 / DO2 •Qs/Qt = ( PA-a O2 ) / ( PA-a O2 ) / ( Ca-v O2 ) - Shunt fraction Pa O2 = partial arterial oxygen pressure. Introduction to Critical Care Intensive Care Medicine Ventilators ARDS Hemodynamic Monitoring Vasoactive Drugs