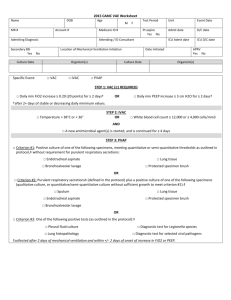
Adult Ventilator Management/Weaning Plan MSJ-00000-176
advertisement

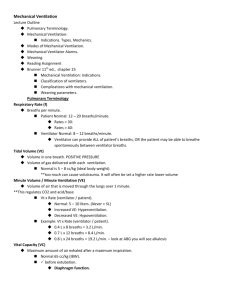
1 Adult Ventilator Management/Weaning Plan MSJ-00000-176-0107 D/C all previous respiratory care orders prior to ventilator plan initiation. Low PEEP Guidelines Adjust PEEP 8-14 cm H20 to maintain ordered SPO2 goal Increase PEEP by 2-3 cm H2O q 10 min to achieve ordered SpO2 goal NOTIFY PHYSICIAN AT PEEP 14 cm H2O Use lower PEEP / higher FIO2 guidelines unless order option indicator for higher PEEP / Lower FIO2 is checked by physician High PEEP guidelines Adjust PEEP 8-18 cm H20 to maintain ordered SpO2 goal Increase PEEP by 2-3 cm H2O q 10 min to achieve ordered SpO2 goal NOTIFY PHYSICIAN AT PEEP 18 cm H2O Use higher PEEP / lower FIO2 guidelines unless order option indicator for lower PEEP / higher FIO2 is checked by physician Guidelines for PEEP / FiO2 adjustments Low PEEP / High Fio2 Scale 0.3 0.4 0.4 0.5 0.5 FiO2 5 5 8 8 10 PEEP 0.6 10 0.7 10 0.7 12 0.7 14 0.8 14 High PEEP / Low FiO2 Scale 0.3 0.3 0.3 0.3 Fio2 5 8 10 12 PEEP 0.4 14 0.4 16 0.5 16 0.5 18 0.5-0.8 20 0.3 14 PEEP/FIO2 ratios as recommended by ARDSNet 0.9 14 0.8 22 0.9 16 0.9 22 (www.ardsnet.org) Maintain Plateau Pressure < 30 cm H2O Sensitivity trigger flow 0.5 – 2.0 liters/minute OR pressure less than 3.0 cmH2O All Vt calculations to be made on Predicted Body Weight determination. Calculate predicted body weight (PBW) Males = 50 + 2.3 [height (inches) - 60] Females = 45.5 + 2.3 [height (inches) -60] 0.9 18 1.00 18-24 1.00 1.00 22 24 2 Patient is to be placed on initial ordered ventilator mode, mode may be adjusted as appropriate, and weaned per reference txt guidelines. (excluding high frequency ventilation) 1. Mandatory Assist Control (AC) Pressure Controlled Ventilation (PCV) a. Initial settings Inspiratory pressure (above PEEP) to give Vt 5-8 cc/kg/PBW Ti (inspiratory time) 1-3 sec I:E ratio 1:1 - 1:4 Set Respiratory Rate 8-35 b. Weaning parameters Decrease set RR to maintain current minute volume as tolerated 1. Decrease inspiratory pressure and PEEP 2. Slowly decrease mean airway pressure to prevent atelectasis 3. with decreased settings maintain 5-8 cc/kg/PBW FiO2 < 50% PEEP < 10 cm H20 c. Transition patient from PCV/AC to PSV as tolerated 2. Synchronized Mandatory Intermittent Ventilation (SIMV) Volume Control (VC) a. Initial settings Set mandatory Vt 5-8 cc/kg/ PBW I:E ratio 1:1 – 1:4 Set Respiratory Rate 8-35 b. Weaning parameters Decrease set RR to maintain current minute volume as tolerated 1. Decrease PEEP as tolerated to <10 cm H20 2. Decrease mandatory Respiratory Rate as patient tolerates 3. Maintain Vt 5-8 cc/kg/PBW FiO2 < 50% PEEP < 10 cm H20 c. Transition patient from SIMV/VC to PSV as tolerated 3. Spontaneous Pressure Support Ventilation (PSV) a. Criteria Spontaneous RR FiO2 <60% b. Initial settings 5-25 cm H2O Vt (supported) 5-8 cc/kg/PBW or equal to target Vt (mandatory) c. Weaning parameters d. Continue to wean PS Q3-6 hours by 2-3 if spontaneous VT is > 5 cc/kg/PBW Reference text for SBT 4. Bi-level Ventilation 3 a. Initial settings High PEEP Adjust for Vt 5-8 cc/kg/PBW Low PEEP as ordered: 1. high PEEP guidelines 8-18cm H20 2. low PEEP guidelines 8-14 cm H20 Rise time % start at 80% Th (time at high PEEP) 1.2 - 3 sec. Maintaining I:E 1:1 – 1:4 Set PS for total pressure to equal high PEEP + 2 cm H2O 1. low PEEP + PS equal high PEEP + 2 cm H2O Respiratory rate 8-35/minute b. Weaning parameters RR less than 10 to maintain adequate minute volume Th to 1.2 sec. or less Decrease high and low PEEP simultaneously 1. Slowly decrease mean airway pressure to prevent atelectasis 2. with decreased settings maintain 5-8 cc/kg/PBW FiO2 less than 40% Low PEEP less than 10cm H2O c. Transition patient from Bi-Level to PSV when above parameters are met. 5. Bi-level Ventilation / Airway Pressure Release Ventilation (APRV) a. Criteria Acute respiratory distress syndrome FiO2 > 50% PEEP > 10 cm H2O b. Initial Settings Mandatory Breaths 5-12 /minute High PEEP 1. Same as plateau pressure on previous mode 2. Maximum of 30cmH2O Low PEEP 1. 0 cm H2O T low 1. 0.6 to 0.8 seconds 2. 40% of peak expiratory flow a. Airtrap 50 – 75% of exhaled gas b. COPD airtrap 25 - 50% c. Spontaneous Breaths Spontaneous breathing is at LEAST 10% of total minute ventilation 6. Recruitment Maneuver NOTIFY PHYSICIAN a. PSV Mode b. PEEP 40 c. PSV 0 d. Maintain for 40 seconds Notify physician for the following conditions: 1. Difficulty achieving oxygenation or peak pressure goal with above parameters 4 2. New onset sustained FiO2 requirement > 60% 3. Plateau pressure (PpLT) > 30 4. PEEP requirement > 14 cm H2O Low PEEP guidelines 5. PEEP requirement > 18 cm H2O High PEEP guidelines 6. Set ventilator rate >35 7. Spontaneous respiratory rate > 35 8. Unable to achieve adequate Vt in selected mode with PIP pressures < 35 cm H2O 9. Inverse I:E ratio is required 10. Advanced mode change required Monitoring, transports and standards of care 1. ETCO2 monitoring for patients on paralytic drips, ICP monitoring, Neuromuscular Agents, and traumatic brain injury. Adjust ventilator settings as appropriate prior to the Neuromuscular administration. 2. PEEP value on Bag-Valve mask to match PEEP on ventilator 3. Plateau pressures and lung compliance monitoring once a shift and with pertinent ventilator changes. 4. Transport ventilator to be utilized on all transports. 5. OR elevator to be used for all ventilated patients if available. 6. Patients requiring transport to the OR on PEEP setting greater than 10 cm H2O or Bilevel/pressure control ventilation will be taken to the OR and kept on the transport ventilator until transferred to the anesthesia ventilator. SBAR handoff will be given upon patient transfer to anesthesia. Post intervention, Respiratory Therapy will be contacted with (SBAR) handoff to transport the patient from the OR to the ICU at the request of anesthesia/physician. 7. Apply heated circuit if patient temperature is less than 95 ° F 8. Maintain cuff pressure @ or below 30 cm H2O Medications: Albuterol 8 puffs in line every 15 minutes PRN tachypnea/wheezes Albuterol/Ipratropium (Combivent) 8 puffs in line every 2 hours PRN tachypnea/wheezes if currently taking at home and physician order. Call physician if additional puffs required Diagnostics: PCXR: A. STAT: Clinical reason, ETT placement (If not already ordered prior to ventilator plan initiation) ABG: A. Approximately one hour after initiating ventilator support B. Obtain STAT ABG PRN if there is a sudden clinical deterioration 5 General Weaning Guidelines please see mode specific weaning parameters: 1. 2. 3. 4. 5. 6. Titrate ventilator to PSV Wean to maintain RR less than 24 Minute ventilation at baseline FiO2 less than 50% PEEP equal to 8cm H2O Adjust PS to maintain Vt 5-8 cc/kg/PBW Spontaneous Breathing Trial: 1. Coordinate with Nursing staff the pairing of the spontaneous breathing trial (SBT) and sedation awakening trial (SAT). 2. Screen and document the exclusion criteria for not performing an SBT as listed below: FiO2 greater than 50% Patient on paralytic PEEP greater than 8 cm H2O pH less than 7.3 Patient not arousable. Hemodynamically unstable Physician ordered Active seizures Abnormal intracranial pressure Active ETOH Tracheostomy 3. Inform nurse of initiation of SBT 4. Once daily, place patient on: Current FiO2 (less than or equal to 50%) PEEP 5 cmH2O PSV = 5cmH2O for 8.0 or larger ETT PSV = 8 cmH2O for 7.5 or smaller ETT 5. Trial duration 30 - 120 minutes 6. Calculate and document RSBI: Spontaneous RR / Spontaneous Vt in Liters 7. Observe and terminate SBT for the following signs of decomposition. If RR/Vt (L) is > 100 in first 5 minutes, return to prior vent settings. Tachycardia >130 or Bradycardia < 60 RR > 30 or < 8 for greater than 5 minutes SpO2 < 88% Respiratory Distress 6 Mental status change Acute cardiac arrhythmia 8. Completion of SBT Obtain ABG at completion of spontaneous breathing trial if condition warrants. If patient fails spontaneous breathing trial, return to prior vent settings. If patient passes spontaneous breathing trial (tolerates 30-120 minute spontaneous breathing trial, based on stable vital signs, SpO2, RR < 25), notify physician to obtain extubation order. Prior to attempted extubation, assure patient able to cough, deep breath and participate in pulmonary care Deflate ETT cuff and assure air movement around tube. Notify physician if no air movement before proceeding with extubation Initiate Adult Medical Surgical or Trauma Extubation Protocol Plan upon extubation order. CVICU post surgical extubated < 24 hours initiate CV extubation protocol. Ventilator weaning to tracheostomy collar trials postoperative tracheotomy Immediately upon tracheotomy tube placement, the patient will be evaluated by RT and RN for initiation of the Adult Ventilator/Tracheotomy weaning path. The team will then communicate the appropriateness of trach collar trials prior to the weaning procedure. The Physician may option out of trach collar trial criteria by unselecting the pre-checked trach collar order on the ventilator management plan. Procedure: 1. Initial Ventilator Weaning Titrate ventilator support to spontaneous mode and PSV. Wean FIO2 as tolerated to maintain SPO2 greater than 92%. Wean PEEP to 8 cmH2O Adjust PSV to maintain Vt at 5-8 cc/kg/PBW or lowest appropriate pressure for patient comfort and minimal work of breathing. 2. Patient evaluation for trach collar trial Ventilator settings weaned as per above guidelines. Sedation evaluation for minimal levels or coordination of SAT to facilitate SBT. Perform SBT. (See RSBI criteria in ventilator management plan). If RSBI is < 105 after 30 minutes proceed to trach collar trial. If RSBI is > 100 in the first 15 minutes, return to previous ventilator settings and reevaluate q day until criteria is met to continue with trach collar trail. 3. Tracheostomy collar trial exclusion criteria Systolic BP < 90 mm HG on vasopressors Systolic BP < 90 mm HG and Heart Rate < 50 or > 130 bpm Temperature > 100.4 FIO2 > 50% or PEEP greater than 8 cm H20 and unable to wean. 7 RR greater than 30 breaths per minute with increased work of breathing and prominent accessory muscle use. Traumatic/Ischemic brain injury patients with baseline tachypnea will be assessed for continuation of trach collar trials upon MD direction. SPO2 < 90% on current ventilator setting. Spontaneous Vt < 0.3 Liters unless normal for patients ideal body weight. P/F ratio less than 200 on FIO2 > 50% and PEEP of 8 cm H2O or greater. Weaning to Trach Collar trial At anytime during the Trach collar trial the Respiratory Therapist may place patient back on previous ventilator settings as set criteria and patient condition dictates. ABGs may be obtained for evaluation of patient status or clinical deterioration during the procedure. Physician will be communicated as to the results of all trials and ABGs. Procedure: Trach Collar Trial 1. Place patient on tracheostomy collar with cool aerosol 2. EZPAP Q4 while off ventilator 3. Begin FiO2 at same percentage as the set ventilator FiO2 and titrate to maintain SPO2 >90%. If a FiO2 of > 60% is required to maintain Spo2 > 90, place back on ventilator at previous settings. Re-evaluate and continue to attempt trachestomy collar trials BID until patient can sustain an SPO2 > 90% on a set FIO2 < 60%. At any time during the tracheostomy collar trial an FIO2 of greater than 60% is required to maintain an SPO2 of 90% the patient will be placed back on the ventilator at the previous settings. 4. Continue Trach collar trial as patient tolerates utilizing the following schedule. Initial 24 hours Trach collar goal 4-6 hours BID as patient tolerates and rest 2-4 hour between each trial. At anytime during the initial 4-6 hour trial the patient fails place back on previous ventilator settings. Attempt a second trial after 4 hours of rest on the ventilator. Use the timeframe that was established during the first trial as a baseline goal for the second attempt. 8 Example: If patient tolerates first trial for 35 minutes then set the goal for the second trial at 35 minutes. Extend as tolerated up to 4-6 hours. The RCP may draw ABGs as needed for sudden deterioration and evaluation for continuation of initial tracheostomy collar trails if assessment dictates the need. Difficult wean patients will be evaluated and traceostomy collar trials will be adjusted to patient tolerance and extended by one to two hours BID based on the weaning assessment tool below. Post 24 hours Extend patient trach collar trials as tolerated up to 16 hours and rest on ventilator as needed. If patient is comfortable and wishes to continue the trial, extend trach collar trials as condition permits. Re-evaluate patient status as needed for return to ventilator for rest. Post 48 hours Extend trach collar trials to 24 hours and rest on ventilator as needed. Weaning Assessment *Assess patient for new onset fatigue or instability and place patient back on the ventilator at previous settings. Tachycardia > 130, Bradycardia < 60 or a 20 % change in heart rate from base line. RR > 30 or < 8 for greater than 15 minutes. Excluding traumatic/Ischemic head injury patients with MD order to continue trial. SPO2 < 90% on set FIO2 > 60% Mental status or LOC changes. Acute cardiac arrhythmia or sudden hemodynamic instability. RR greater than 30 breaths per minute with increased work of breathing and prominent accessory muscle use. All trach collars will be humidified via cool aerosol low flow system. Heat may be added to the system upon a physician / provider order or evidence of thick, retained secretions is present. Trach collars will be monitored and documented a minimum of every 4 hours. The patient will be observed for signs of de-compensation including HR, RR, Breath sounds, Hemodynamic stability, SpO2, and level of fatigue. Respiratory medications given via the ventilator will be continued when the patient is on trach collar trials either by metered dose inhaler via bag-valve, or nebulizer as appropriate.