MODES OF MECHANICAL VENTILATION
advertisement

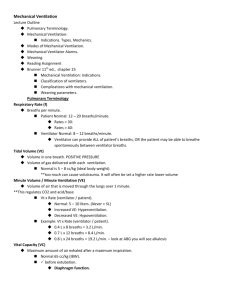
Educational Resources PICU resident handbook with relevant PICU topics is available at http://peds.stanford.edu/Rotations/picu/pic u.html Hard copy is available in the resident call room. PICU chapters at http://peds.stanford.edu/Rotations/picu/picu.html Monitors in ICU Vascular Access Codes ICP management Status Epilepticus Sedation Pediatric Airway Airway Management Mechanical Ventilation ARDS Status Asthmaticus Inotropes Shock Sepsis Meningococcus PICU chapters at http://peds.stanford.edu/Rotations/picu/picu.html Cardiomyopathy Liver Failure Acute Renal Falilure Fluids, Electrolytes, Nutrition Oncology Transfusions DKA Submersion Injuries Brain Death End of life issues PICU Tables at peds.stanford.edu Sedation Inotropes Shock MECHANICAL VENTILATION SARASWATI KACHE, M.D. Clinical Assistant Professor Spontaneous respiration vs. Mechanical ventilation Natural Breathing Negative inspiratory force Air pulled into lungs Mechanical Positive Ventilation inspiratory pressure Air pushed into lungs Initiate Mechanical Ventilation Hypoxia Hypercarbia Airway protection (Decrease demand in cases of poor cardiac output) Ventilators: a Schematic IMPORTANT TERMS TIME Volume Amount of tidal volume that a patient receives Pressure I - Time: amount of time spent in inspiration E - Time: amount of time spent in expiration Measure of impedance to gas flow rate Flow Measure of rate at which gas is delivered A Few More Terms PEEP = positive end expiratory pressure Pressure maintained in the airways at the end of exhalation Keeps Alveoli from collapsing PIP = peak inspiratory pressure Point of maximal airway pressure Delta P = the difference between PIP – PEEP MAP = mean airway pressure ICU Ventilator: Evita 4 ICU Ventilator: Evita 4 Types of Ventilation …. Compliance = Volume Pressure Volume Ventilation Preset Volume PEEP Rate I-time FiO2 Ventilator Determines Pressure required Advantages Guaranteed minute ventilation More comfortable for patient Draw-backs Large ETT leak Not optimal for poorly compliant lungs Pressure Ventilation Preset PIP PEEP Rate I-time FiO2 Vent determines Tidal volume given Advantages Provides more support at lower PIP for poorly compliant lungs Draw back Minute ventilation not guaranteed Volume vs. Pressure Amount of support to give… MODES OF VENTILATION Controlled Mechanical Ventilation (CMV) Assist Control (AC) Continuous Positive Airway Pressure (CPAP) Intermittent Mandatory Ventilation (IMV) Synchronized Intermittent Mandatory Ventilation (SIMV) Pressure Support Volume Support Pressure Regulated Volume Control (PRVC) Assist Control Volume or Pressure control mode Parameters to set: Volume Rate – time FiO2 I or pressure Assist Control Machine breaths: Delivers Patient’s the set volume or pressure spontaneous breath: Ventilator delivers full set volume or pressure & I-time Mode of ventilation provides the most support SIMV Synchronized intermittent mandatory ventilation Volume or Pressure mode Parameters set: Volume or pressure Respiratory rate I – time FiO2 Pressure support SIMV Synchronized intermittent mandatory ventilation Machine breaths: d Patient’s spontaneous breath: Delivers the set volume or pressure Set pressure support delivered Mode of ventilation provides moderate amount of support Works well as weaning mode Pressure Support Parameters Pressure set: support, FiO2 Machine breaths: none ***** Patient’s spontaneous breaths: set pressure support delivered Purposes: Final step prior to extubation Re-train muscle strength Continuous Positive Airway Pressure (CPAP) Positive airway pressure maintained throughout respiratory cycle: during inspiratory and expiratory phases Can be administered via ETT or nasal prongs Managing the Patient… Pulmonary Compliance Compliance = Volume Pressure Monitor patient’s clinical changes i.e. as compliance improves Volume mode: required pressure decreases Pressure mode: generated volume increases Hypoxia Hypoventilation: decreased alveolar ventilation, i.e. CNS depression Diffusion impairment: abnormality at pulmonary capillary bed Shunt: blood flow without gas exchange Intra-pulmonary Intra-cardiac Ventilation-perfusion mismatch: Both dead space and shunt abnormalities Treating Hypoxia Increase FiO2: >60% toxic to lung parenchyma Increase mean airway pressure PEEP PIP I-time : not too much, not too little Hypercarbia Decreased minute ventilation Respiratory rate Tidal volume Treatment: Increase respiratory rate: assure I-time not too short as rate increased Increase tidal volume Allow permissive hypercarbia Pulmonary Disease: Obstructive Airway obstruction causing increase resistance to airflow: e.g. asthma Optimize expiratory time by minimizing minute ventilation Bag slowly after intubation Don’t increase ventilator rate for increased CO2 Pulmonary Disease: Restrictive Compromised lung volume: Intrinsic lung disease External compression of lung Recruit alveolia, optimize V/Q matching Lung protective strategies High PEEP Pressure limiting PIP: 30-35 cmH2O Low tidal volume: 4-8 ml/kg FiO2 <60% Permissive hypercarbia Permissive hypoxia High Frequency Oscillatory Ventilation HIFI - Theory Resonant frequency phenomena: Lungs have a natural resonant frequency Outside force used to overcome airway resistance Use of high velocity inspiratory gas flow: reduction of effective dead space Increased bulk flow: secondary to active expiration HIFI - Gas Transport Conventional bulk flow Coaxial flow: different flow directions in central and peripheral air columns Taylor dispersion: gas molecules disperse beyond the bulk flow front HIFI - Gas Transport Molecular diffusion: gas mixing within alveoli Pendelluft phenomenon: interalveolar gas mixing due to impedance differences HIFI - Advantages Advantages: Decreased barotrauma / volutrauma: reduced swings in pressure and volume Improve V/Q matching: secondary to different flow delivery characteristics Disadvantages: Greater potential of air trapping Hemodynamic compromise Physical airway damage: necrotizing tracheobronchitis Difficult to suction Often require paralysis HIFI – Clinical Application Adjustable Mean Parameters Airway Pressure: usually set 2-4 higher than MAP on conventional ventilator Amplitude: monitor chest rise Hertz: number of cycles per second FiO2 I-time: usually set at 33% HIFI - Applications Oxygenation Mean airway pressure FiO2 Ventilation Amplitude Hertz I-Time Scenario #1 The following blood gas is presented to you for a 4yr patient that is now 3hours post-op from an OLT. 7.52 / 24 / 250 / 20 / -4 The ventilator settings are SIMV PC/PS PEEP – 4, Delta P-28, FiO2 – 50%, RR – 12. Scenario #2 A 8yr female with ALL s/p chemo presents to the PICU with fever and neutropenia 1day prior. She is found with positive blood cultures this AM and got intubated secondary to respiratory failure. It is now 4am and the morning labs show the following ABG: 7.23 / 60 / 58 / 22 / -2 The ventilator settings are SIMV TV - 10cc/Kg, PEEP – 5, PIP – 38, PS – 14, FiO2 – 70%, RR – 20, I-time – 0.7 You go to examine the patient and she is agitated, hypertensive, and with a respiratory rate of 40. Scenario #3 There is a 6 month old patient that presents with RSV bronchiolitis that progresses to severe disease and the patient is now on a HIFI ventilator. The patient’s ABG is as follows: 7.24 / 58 / 75 / 21 / -3 The ventilator settings are as follows: HIFI with MAP – 20, Amp – 28, Hz – 8, FiO2 – 40%. As you are looking at the chest X-ray, the nurse mentions the patient looks more edematous this evening compared to last night. References http://www.ccmtutorials.com/rs/mv/ Editors: Rogers MC & Nichols DG. Textbook of Pediatric Intensive Care. Baltimore, Willimams & Wilkins, 1996. Cairo JM & Pilbeam SP. Mosby’s Respiratory Care Equipment. St. Louis, Mosby, 1999. Evita 4 Intensive Care ventilator, Operating instructions, 2001. West JB. Pulmonary Pathophysiology. Baltimore, Willims & Wilkins, 1992.