Ulcerative Colitis
advertisement
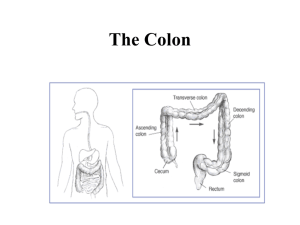
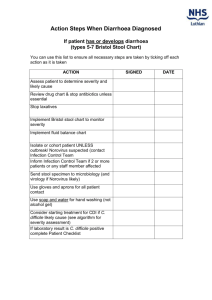
Ulcerative Colitis Commoner than Crohn's disease Recurrent inflammatory disease of the large bowel Always involves the rectum Spreads in continuity proximally to involve a variable amount of the colon. Never spreads beyond the ileocaecal valve ( may get backwash ileitis) Commonest cause of prolonged bloody diarrhoea (outside the Tropics) More common in non-smokers More common in women Cause Unknown Some degree of genetic susceptibility No evidence of infective agent Symptoms Sometimes none Gradual onset (or acute) of rectal bleeding Diarrhoea Abdominal Pain (mimicking GI infection) Proctitis (only rectum involved) Constipation with blood on the stool More extensive disease Severe diarrhoea (nocturnal - with urgency and tenesmus) Weight loss Fever Symptoms of hypoproteinaemia Symptoms of anaemia Fulminant colitis Liquid stool mixed with blood and pus Extra-intestinal manifestations Signs Few if chronic Clubbing Fulminant Fever Tachycardia Hypotension Weight loss Dehydration Tender colon Extra-intestinal manifestations Diagnosis Sigmoidoscopy Red, raw mucosa Contact bleeding Inflammatory 'pseudopolyps' due to confluent ulcers Rectal biopsy Inflammatory infiltrate Mucosal ulcers Crypt abscesses Abdominal X-Ray Colonic dilatation (+/- perforation) in fulminant disease Absent faeces implies involvement Barium enema Fuzzy mucosal margins Pseudopolyps Ulceration If chronic - Colon shortening and loss of haustrae (never do a barium enema if severe - risk of perforation) Stool culture Microscopy Exclude infectious cause Differential Diagnosis Crohn's Ischaemic colitis Infection - Pseudomembranous colitis - Shigella - Campylobacter - E Coli - Cryptosporidium - other if immunocompromised Complications Haemorrhage Dehydration Toxic dilatation Perforation Colon cancer (increased risk with increased duration and extent) - surveillance with frequent biopsies may reveal occult cancers. Liver involvement - e.g. fatty liver, hepatitis, PSC Medical Management Managing Acute Relapses 1. Oral prednisolone 2. Daily steroid enemas 3. Reduce steroids if improving, increase dose if not 4. If systemically unwell - admit to hospital 5. Cyclosporin may be useful (watch renal function) 5-day regimen for Severe Colitis 1. 2. 3. 4. 5. 6. 7. 8. Get expert help. Inform surgeons Nil by mouth. Set up IVI Chart TPR, BP 2xdaily physical examination. Record stool frequency/character Daily: FBC, U&E, plain films, abdominal girth Hydrocortisone IV plus 2 hydrocortisone acetate foam enemas/day Consider IV nutrition. IM vitamins If improved transfer to oral prednisolone after 5 days, plus sulfasalazine. Indications for Colectomy: - Deteriorating colitis after 5 days - 'Toxic' dilatation of colon (megacolon) - Perforation Surgical mortality 2-7% Mortality with perforation 50% Maintaining Remissions Sulfasalazine - lowers relapse rate by 65%. (SE: rash, male infertility, agranulocytosis, folate deficiency) Mesalazine - not as effective, but less side effects Olsalazine - (as Mesalazine) Long term Azathioprine may reduce need for steroids Surgery Proctocolectomy and ileostomy Ileorectal anastomosis Pouch formation Indication: failed medical therapy or complications