IBD - Mosaiced.org
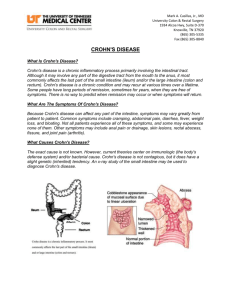
advertisement

IBD – Crohn’s Disease (Gastroenterology): Example case: Definitions: A chronic inflammatory disease of the bowel causing lesions throughout any part of the GIT from mouth to anus. Epidemiology: 150/100,000 Australians Commonly diagnosed between 15-30yoa More common in Western countries Female > male Increases risk of colorectal & small bowel cancer Associated with sclerosing cholangitis in ~10% of ppl Risk/Protective factors: Risk: Smoking Family Hx Other GIT disorders e.g. coeliac, food intolerance Female There are 3 major patterns of involvement in Crohn’s disease including: Disease in the ileum and cecum, occurring in 40% of patients. Disease confined to the small intestine, occurring in 30% of patients. Disease confined to the colon, occurring in 25% of patients. Aetiology/Causes: Unknown cause. Genetic link with 8-10% of sufferers having other family members with Crohn’s while parents with Crohn’s have a 3-5% chance of an offspring with Crohn’s. Disease can be aggravated/stimulated by bacterial infection. Factors believed to influence disease expression: Smoking (x2 ↑ risk) Breastfeeding for >3 months reduces risk Exposure to antibiotics as a child increases risk “hygiene hypothesis” i.e. overly sterile upbringing Crohn’s Normal physiology/anatomy: Pathophysiology: Transmural (across wall) inflammation i.e. layers from the mucosa to muscle level leading to discontinuous lesions (i.e. patches), most commonly affecting the ileum area, but again can affect any part of the GIT. The cause is inappropriate activation of the innate immune system by natural gut flora neutrophil mediation T cell activation cytokine release. Can cause fistulas, scarring, strictures Clinical Features (signs & symptoms): Signs: Ulcers (aphthous mouth) Fistulas – anorectal, enterorectal, enterocutaneous fistulas are most common Liver inflammation – pain, jaundice Pyoderma gangernosum – necrosis of tissue deep ulcer most common in legs Erythema nodosum – painful, red nodules mostly on limbs that last ~2 weeks and can change colour and texture Uveitis/Iritis – inflammation of the uvea (layer of the eye made up of iris, ciliary bodies and choroid) pain, tearing, redness, sensitivity to light and blurred vision. Symptoms: Diarrhoea Rectal bleeding - melena, haematochezia Abdo/rectal pain Tenesmus (constant feeling of needing to defecate) Fatigue/malaise Joint pathology – arthralgia & arthritis, ankylosing spondylitis Neurological – lack of B12 absorption mainly headaches, depression, myopathy, peripheral neuropathy Malabsorption weight loss Fever NB: Crohn’s is less associated with systemic manifestations than UC. All forms of Crohn - Diarrhea occurs in most patients - Abdominal pain in 2/3 - Weight loss, malaise - Abdominal tenderness - Low-grade fever - Abdominal mass (occasionally) - Fistula: Perirectal, bladder, skin, vagina - Extraluminal disease (10%): Skin, iritis, arthritis, sclerosing cholangitis Small-bowel disease only (15-30%) - Diarrhea prominent, including nocturnal - Vague abdominal pain frequent - Intestinal obstruction (1/3): Cramping abdominal pain precedes for months. - Bleeding in 20%, rarely massive - Perianal disease, including fistulae - Internal fistulae Colon disease only (25-30%) - Diarrhea prominent, including nocturnal - Hematochezia - Abdominal pain in 50%, relieved by stooling - Perianal disease in 40%, fistulae - Weight loss prominent - Megacolon in 10% - Intestinal obstruction occasional Colon and small-bowel disease (40-60%) - Intestinal obstruction much more common than in other types DDx: UC – only occurs in mucosa layers of colon and rectum with less extra-intestinal s/s. Appendicitis – if near ileocecal area, RIF pain, fever, fatigue Intermediate colitis PID Endometriosis IBS Ischaemic colitis Infection Diverticulitis Investigations & relevant findings: Magnetic resonance enterography – type of MRI with contrast (usually gadolinium) to produce detailed images of intestine Scopes + biopsy – colonoscopy, sigmoidoscopy, endoscopy – see cobblestone appearance, apthous & linear ulcers, friability Small bowel enema Capsule endoscopy (pillcam) Barium enema – barely used Stool MSC – to exclude infectious diarrhoea Blood tests – inflammatory markers (ESR, CRP), malnutrition (FBE, vitamin levels, iron studies) and gut & liver functions (UEC, LFTs) Serum ASCA (anti-saccharomyces cerevisiae antibodies) +ve in 50% of patients. Treatment/management: Lifestyle – maintaining weight and nutrition (reduce intake of intolerant substances e.g. protein, fats, fibre), relieve stress, quit smoking, reduce alcohol. Drugs o Mild attacks – aminosalicylates (anti-inflammatory drugs) or corticosteroids (prednisolone) PO (per oral) 30mg for 1 wk, then 20mg for 2-4wks, if improved, taper off 5mg/2-4wks, stop when normal again. o Immunosuppresants in patients with frequent relapse o Severe disease – IV steroids (hydrocortisone), nil by mouth, IVI (infusions - saline, dextrose), if improving after 5 days, change to oral prednisolone, if no improvement = infliximab & adalimumab(TNF-α inhibitors) o Antibiotics – metronidazole if infection or perianal disease Surgery – if drug therapy fails or complications occur. Bowel resection, stricturoplasty or closer of fistulae and drainage abscesses can be done. Prognosis: No cure is available, 15% of patients are unable to work after 5-10yrs. Slightly higher mortality rate than normal Complications: Small bowel obstruction Toxic dilatation (>6cm colon diameter) Abscess (buildup of pus and inflammation), fistulae (e.g. colovesical aka. Bladder, colovaginal, perianal etc), perforation, rectal haemorrhage CA colon fatty liver PSC, cholangiocarcinoma renal stones osteomalacia, malnutrition (B12) amyloidosis NB: perianal disease i.e. any condition affecting the rectal/anal area affect 50% of patients.