File - Sheila Mulhern, RDN
advertisement

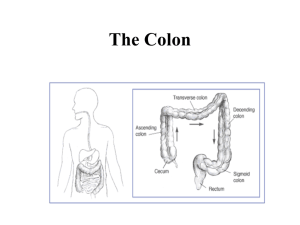
Ulcerative Colitis Sheila Mulhern & Stephanie Howard Overview & Statistics • Irritable Bowel Disease (IBD) is a chronic condition of immune response and inflammation of the GI tract • Two most common forms are ulcerative colitis and Crohn’s disease • Ulcerative colitis is a chronic disease of inflammation affecting the lining of the colon and the rectum • More than 1.5 million Americans have Crohn's disease or ulcerative colitis, the most common forms of inflammatory bowel disease. • Video http://www.youtube.com/watch?v=FjUke8TMwhU&feature=r elated CDC Statistics • IBD doesn’t have a medical cure and commonly requires a lifetime of care • IBD is one of the five most prevalent gastrointestinal disease burdens in the US • IBD has an overall health care cost of more than $1.7 billion • IBD accounts for more than 700,000 physician visits, 100,000 hospitalizations, and disability in 119,000 patients in the US Ulcerative Colitis Is a chronic Inflammatory Bowel Disease (IBD) which only affects the lining of the colon The lining of the colon becomes inflamed and develops tiny open sores, or ulcers that produce pus and mucus Digestive Functions Structure Activity Functions Lumen Bacterial activity Breaks down undigested nutrients to be expelled as feces or absorbed and detoxified in liver; synthesizes certain B vitamins and vitamin K Mucosa Secretes mucus Lubricates colon and protects mucosa Solidifies feces and contributes body’s water balance Absorption Muscularis Haustral Churning Peristalsis Mass peristalsis Defecation reflex Series of muscular contractions that moves the contents through large intestines to rectum for elimination Etiology • The exact cause of ulcerative colitis is unknown, proposed causes includes; genetics, immune reactions and environmental factors • Genetically susceptible individuals have abnormalities of humoral and cell-mediated immunity or generalize enhanced reactivity against commensal intestinal bacteria and this deregulated mucosal immune response predisposes these individuals to colonic inflammation • Immune reactions to foreign substances (antigens) that stimulate the bodies defense to produce inflammation that continues without control progressing into IBD/UC • Environmental factors such as sulfate-reducing bacteria which produce sulfides, are found in large numbers of patients with UC than in other people Clinical Manifestations • Ulcerative Colitis (UC)symptoms may vary depending on the severity of inflammation or its location • For therapeutic and prognostic purposes, Doctors usually classify UC according to its location and presentation • The severity of the symptoms often correlates with the anatomic extent of the disease, another parameter that will guide treatment • The Mayo scoring system is one instrument that has been used to judge disease severity and monitor patients during therapy. • Scores range from zero to 12, with higher scores correlating with more severe disease. Ulcerative Colitis Symptoms • Half of the patients have mild symptoms, others have more severe attacks that occur often. • Symptoms vary in severity and may start slowly or suddenly • Bowel movements become looser and more urgent • Persistent diarrhea accompanied by abdominal pain and blood in the stool • Tenesmus (rectal pain) • Bloody stool • Crampy abdominal pain • Loss of appetite • Weight loss • Low energy and fatigue • Children suffering with UC may have delayed growth and development Other UC Symptoms • • • • • • Fever Gastrointestinal bleeding Joint pain and swelling Mouth sores (ulcers) Nausea and vomiting Skin lumps or ulcers Possible Complications of Ulcerative Colitis • • • • • • • • • • • Severe bleeding Anemia Malabsorption of nutrients Perforated colon (hole in colon) Severe dehydration Kidney stones Liver disease (rare) Osteoporosis Inflammation of skin, joints and eyes Increase risk of colon cancer Rapidly swelling colon (toxic megacolon) Risk Factors • Sex According (The Crohn’s and Colitis Foundation of America) UC is more common in women than men, but the Mayo Clinic studies found Ulcerative Colitis to be about equal • Age UC occurs at any age, but most often in the 30’s with a second peak in the 50’s and 60’s • Race or ethnicity UC affects all ethnic groups, but more common in Caucasians and Ashkenazi Jewish descent • Family History You’re at a higher risk if you have first degree family members (parents, siblings, child etc.) • Medications have been cited as possible linked to UC, such as Isotretinoin use to treat scarring cystic acne that doesn't respond to other treatments. Sold under brand names Accutane, Amnesteem, Claravis and Sotret, also Tetracycline. Goals of Treating UC • • • • • • Induce and maintain remission Prevent reoccurrence Control impact of complications Improve nutritional status Improve quality of life Correct with surgery if necessary Understanding Quality of Life • • • • May avoid travel or activity Fear of being in public Limited social interaction Needs to plan ahead for bathroom locations, medications or personal supplies • May resist exercise • Avoidance of foods • Support group: Crohn’s and Colitis Foundation of America (CCFA) UC vs. Crohn’s Disease In UC, inflammation is limited to the colon and continuous. In Crohn’s disease inflammation can occur anywhere along the GI tract, most common areas are the terminal ileum and the colon. Pattern is patchy. UC vs. Crohn’s Disease Comparison factor UC CD Type of IBD Yes Yes Prevalence About equal About equal Area affected Colon Lesions Shallow ulcerations Colon and small intestine Deep ulcerations Ulceration pattern Continuous, snake-like Patchy Surgical option 25-40% will ultimately have surgery 66-75% will eventually undergo surgery Colorectal cancer risk Higher than CD Lower than UC Abnormal Colonoscopy Results Analysis Diagnosis: Tests for Ulcerative Colitis • Colonoscopy with biopsy is used to diagnose UC • Other tests which can supplement diagnosis – Barium enema – Fecal sample – Complete blood count (CBC) – C-reactive protein (CRP) – Sedimentation rate (ESR) Treatment: Medications • Anti-inflammatory – first step in treatment – Sulfazine (Azulfidine), Mesalamine (Asacol, Lialda), Corticosteroids (prednisone) • Immune System suppressors – reduce inflammation by targeting immune system response – Azathioprine (Azasan, Imuran), Mercaptopurine (Purinethol), Cyclosporine (Gengraf, Neoral), – Infliximab (Remicade) – blocks inflammatory pathways • Additional medications: – Antibiotics, anti-diarrheal, mild pain relievers (Tylenol/ acetaminophen; excludes Advil, Motrin, aspirin), iron supplements Treatment: Surgery • Surgery needed if medication treatment is unresponsive • The CCFA estimates this option is used for 2540% of cases • Surgery is considered a cure – two main options – Proctocolectomy ileostomy – Ileoanal anastomosis Treatment: Surgery Proctocolectomy Ileostomy • Removal of the large intestine and rectum, leaving the lower end of the small intestine (the ileum). • The anus is sewn closed and the doctor makes a small opening called a stoma in the skin of the lower abdomen. • The ileum is connected to the stoma, creating an opening to the outside of the body. The surgery that creates the opening to the intestine is called an ileostomy. • Stool empties into a small plastic pouch called an ostomy bag that is applied to the skin around the stoma. The bag is emptied several times a day. Proctocolectomy Ileostomy •Hospital stay ranges from several days to two weeks after surgery •For those who can’t tolerate anesthesia for long periods (age, illness) Treatment: Surgery Ileoanal anastomosis – Some or all of the colon and the diseased lining of the rectum is removed. – The end of the small intestine (the ileum) is connected to the anal canal. This allows bowel movements without an ostomy. Proctocolectomy vs Ileoanal Anastomosis Nutritional Risks • • • • • Malabsorption, maldigestion Dehydration Protein deficiency, loss of lean muscle mass Vitamin and mineral deficiencies Vitamin D and calcium deficiency, risk for osteopenia and osteoporosis Guidelines for Medical Nutrition Therapy • Energy needs of UC patients are not generally increased – Disease increases BMR and physical activity decreases • Protein requirements may be increased – Inflammation treatment drugs induce negative nitrogen balance and cause a loss of lean muscle mass – Additional protein loss in ulcers and tissue damage from disease – Increase protein 1.3-1.5 g/kg/day • Supplements of omega fatty acids – Shown to reduce disease activity for inflammation and immune response Guidelines for Medical Nutrition Therapy • Reduce excessive intake of lactose, fructose and sorbitol – may contribute to abdominal cramping, gas and diarrhea • Avoid foods that are not well tolerated • Use foods containing prebiotics and probiotics – Findings are still being investigated but many show beneficial bacteria is introduced and reduces chemicals causing inflammation – Some studies didn’t show a difference when a placebo was used – Studies still trying to show whether they actually alter GI microflora and immunologic response in the gut Guidelines for Medical Nutrition Therapy • Supplements needed – folate, B6, B12, minerals and trace minerals – Replace those lost due to maldigestion, malabsorption, drug-nutrient interaction or inadequate intake – Folic acid needed to digest protein • Supplements needed – zinc, potassium, selenium – Due to aggravation from diarrhea • Supplements of vitamin D and calcium – Due to intermittent corticosteroids (inflammation/ immune) – Find alternate sources: fortified soy milk, fortified juices, yogurt – At risk for osteopenia and osteoporosis • Reduce fiber intake, moderate as needed • Enteral formula or parenteral nutrition if necessary Guidelines for Medical Nutrition Therapy • Eat several small meals instead of three large meals • Avoid caffeine, alcohol, fried, spicy intake • Avoid gas forming, sulfer containing foods – lactose, eggs, carbonated beverages, certain vegetables and fruit • Drink plenty of fluids • Low residue – More refined grains, white pasta, white rice, soluble fiber (oatmeal, applesauce – no sugar added) – Avoid tough, fibrous fruits (pineapple), vegetables, whole grain breads, celery – Reduce fiber to 10 g fiber a day; high fiber is 20-35 g/day – Slowly add fiber back to diet Diet Planning: Post-surgery • • • • • • • Name: Mr. Goldstein Age: 44 Weight: 195 lbs. Height: 5' 10" Gender: Male BMI: 28 Activity Level: Sedentary (post-surgery) Diet Planning: Post-surgery Menu Breakfast • • Egg White, Cheddar Cheese, Shredded, 0.25 c, Spinach, Chopped, Boiled, Drained 0.5 c., Cranberry Juice Drink with Vitamin C Added 8 fl. oz. Kellogg’s Rice Krispies Cereal 1.5 c., Soy Milk, Calcium Fortified 8 fl. Oz. Lunch • • Low Fat Plain Yogurt 1 c, Grape Juice, Unsweetened, with Added Vitamin C 8 fl. oz. Plain English Muffin, Enriched, Toasted, Peanut Butter, Smooth 2 T., 0.5L water Dinner • • • Tilapia, baked or broiled 100 g, Whole Green Beans, Canned 0.5 c., Long Grain White Rice, Enriched, Parboiled, Cooked 0.5 c. Tilapia, baked or broiled 100 g, Mixed Vegetables, Canned 0.5 c., Boston Market Home-style Mashed Potatoes 0.75 c. 1L water Snacks • • • Applesauce, Unsweetened, Canned 0.5 c. Lucerne No Salt Added 1% Fat Cottage Cheese 0.5 c. Oatmeal, Cooked with Water 1 c. Diet Analysis: Post-surgery Recommended Yours Carbohydrates 45%-65% 949-1371 kCal 53% 1133 kCal Proteins 10%-35% 211-738 kCal 25% 539 kCal Fats 20%-35% 422-738 kCal 22% 479 kCal Diet Analysis: Post-surgery Energy Kilocalories 2109 kcal, 2142.22 kcal, 102% Carbohydrate 237 - 343g, 287.97 g Fat, Total 47 - 82g, 54.07 g Protein(g/kg/day) 70.76 g, 134.63 g, 190% Fat Saturated Fat < 10%, 21.89 g Monounsaturated Fat, 16 g Polyunsaturated Fat, 10.4 g Cholesterol 300 mg, 188.36 mg, 63% efa Omega-6 Linoleic, 17 g, 8.69 g, 51% Omega-3 Linolenic, 1.6 g, 0.7 g, 44% Carbs Dietary Fiber, Total 38 g, 19.7g, 52% Sugar, Total, 131.61 g Diet Analysis: Post-surgery Other Water, 3.7 L, 3.03 L, 82% Alcohol, 0 g Vitamins Thiamin, 1.2 mg, 1.7 mg, 142% Riboflavin, 1.3 mg, 2.8 mg, 215% Niacin, 16 mg, 28.93 mg, 181% Vitamin B6, 1.3 mg, 2.05 mg, 157% Vitamin B12, 2.4 mcg, 9.89 mcg, 412% Folate (DFE), 400 mcg, 658.8 mcg, 165% Vitamin C, 90 mg, 196.02 mg, 218% Vitamin D (ug), 5 mcg, 3.92 mcg, 78% alpha-tocopherol (Vit E), 15 mg, 7.41 mg, 49% Vitamins Vitamin A (RAE), 900 mcg, 956.91 mcg, 106% Vitamin A (IU), 3000 IU, 12670.48 IU, 422% Minerals Calcium, 1000 mg, 1425.45 mg, 143% Iron, 8 mg, 17.44 mg, 218% Magnesium, 420 mg, 427.1 mg, 102% Potassium, 4700 mg, 3280.19 mg, 70% Zinc 11 mg, 11.33 mg, 103% Sodium 1500 mg 3042.59 mg 203% Resources • • • • • • • • • Krause’s Food and Nutrition Care Process, 13th edition UC image - Monroe Carell Jr. Children's Hospital at Vanderbilt http://www.childrenshospital.vanderbilt.org/services.php?mid=5806 PubMed colonoscopy image http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001296/ Barium enema image http://www.emedicinehealth.com/script/main/art.asp?articlekey=138576&ref=128928 Colonospocy abnomalities image http://www.tabletprep.com/colonoscopy/index.aspx MayoClinic http://www.mayoclinic.com/health/ulcerative-colitis/DS00598 MayoClinic, UC medications http://www.mayoclinic.com/health/ulcerativecolitis/DS00598/DSECTION=treatments-and-drugs John’s Hopkin’s surgery images http://www.hopkinsgi.org/GDL_Disease.aspx?CurrentUDV=31&GDL_Cat_ID=AF793A59-B736-42CB-9E1FE79D2B9FC358&GDL_Disease_ID=b329650a-f196-4b6e-89d2-1d9bae11538b Print out for students http://www.tabletprep.com/docs/colonoscopy.pdf References • • • • • http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001296/ http://ibdcrohns.about.com/od/ http://www.ccfa.org/assets/pdfs/ulcerative-colitis-the-a-to-z.pdf http://emedicine.medscape.com/artoc;e/183084-0verview http://www.mayoclinic.com/health/ulcerative-colitis/DS00598/METHOD=print