Intestinal Ischemia
advertisement
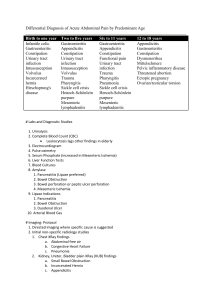
Intestinal Ischemia Michele Young, MD Chief GI Phoenix VA Hospital Banner/VA GI Fellowship Program Director Outline • • • • • • • • • Types Anatomy Pathophysiology Acute Mesenteric Ischemia Mesenteric Vein Thrombosis Focal Segmental Ischemia Colon Ischemia Chronic Mesenteric Ischemia Vasculitides Types TYPE FREQUENCY (%) Colon ischemia 75 Acute mesenteric ischemia 25 Focal segmental ischemia <5 Chronic mesenteric ischemia <5 Anatomy – Celiac Axis • Supplies stomach, duodenum, pancreas, and liver • Three branches: left gastric, common hepatic, splenic • Common hepatic: gastroduodenal, right gastroepiploic, anterior superior pancreaticoduodenal • Splenic: pancreatic and left gastroepiploic Anatomy – Celiac Axis Anatomy – Superior Mesenteric Artery (SMA) • Anterior and posterior inferior pancreaticoduodenal • Middle colic • Right colic • Ileocolic Anatomy - SMA Anatomy – Inferior Mesenteric Artery (IMA) • • • • • Left colic Sigmoid branches Superior rectal Supply distal transverse to proximal rectum Distal rectum: internal iliac Anatomy - IMA Pathophysiology • Bowel can tolerate 75% reduction of blood flow and oxygen consumption for 12 hours • Collaterals open immediately • After hours, vasoconstriction reduces collateral flow (NOMI) • Hypoxia, reperfusion injury ▫ ROS by xanthine oxidase ▫ Microvascular injury by PMNs Acute Mesenteric Ischemia CAUSE FREQUENCY (%) SMA embolus 50 Nonocclusive mesenteric ischemia 25 SMA thrombosis 10 Mesenteric venous thrombosis 10 Focal segmental ischemia 5 Clinical Features • • • • • Acute abdominal pain in patient with CV risks Rapid and forceful bowel evacuation (SMAE) Pain out of proportion to exam Some more indolent (MVT) Unexplained abdominal distention (sign of infarction) or GI bleeding (NOMI) • Physical findings worsen with progressive loss of bowel viability • Infarction: 70-90% mortality Diagnosis • Labs ▫ ▫ 75% have WBC > 15 50% have metabolic acidosis • Plain films ▫ ▫ ▫ ▫ Poorly sensitive (30%) and nonspecific Formless loops of small intestine Ileus, thumbprinting, pneumatosis Portal or mesenteric vascular gas • CT ▫ ▫ ▫ ▫ Colon dilatation Bowel wall thickening Lack of enhancement of arterial vasculature Ascites • CT angiography ▫ Better evaluation of vessels • Selective mesenteric angiography ▫ Gold standard • Prompt laparotomy if angiography not available Portal Gas Treatment • General ▫ Resuscitation, Broad-spectrum antibiotics • Superior Mesenteric Artery Embolus ▫ Cardiac origin ▫ Major: proximal to ileocolic Intra-arterial papaverine Surgical revascularization ▫ Minor and no peritoneal signs Intra-arterial papaverine (or thrombolytics) Anticoagulation SMA Embolus Pre and post treatment Treatment • Nonocclusive Mesenteric Ischemia ▫ Vasoconstriction from preceding cardiovascular event ▫ Angiography Narrowing of SMA branch origins Irregularities in intestinal branches Spasm of arcades Impaired filling of intramural vessels ▫ SMA infusion of papaverine for 24 hours ▫ Surgery if peritoneal signs are present NOMI Pre and post treatment Treatment • Acute Superior Mesenteric Artery Thrombosis ▫ Severe atherosclerotic narrowing ▫ Often superimposed on chronic mesenteric ischemia ▫ Demonstrated on aortography ▫ Management same as SMA embolism Mesenteric Vein Thrombosis • Age: mid-60s to 70s • 20% mortality • Manifest as colon ischemia, acute mesenteric ischemia, or focal segmental ischemia • Causes ▫ ▫ ▫ ▫ Arterial hypertension Neoplasms Coagulation disorders Estrogen Mesenteric Vein Thrombosis • Acute ▫ Pain out of proportion to exam, n/v ▫ Lower GI bleeding suggests infarction • Diagnosis ▫ CT is study of choice (finds >90%) ▫ Mesenteric arteriography Slow or absent filling of mesenteric veins Failure of arterial arcades to empty Prolonged blush in involved segment • Treatment ▫ Incidental: up to six months of anticoagulation (AC) ▫ Peritonitis: surgery, papaverine, post-op heparin ▫ No peritoneal signs: heparin followed by 3-6 mos AC Mesenteric Vein Thrombosis • Subacute ▫ Abdominal pain for weeks to months but no infarction • Chronic ▫ Asymptomatic ▫ May develop GI bleeding from varices ▫ Treatment: control bleeding Focal Segmental Ischemia • Involves small bowel • Causes ▫ ▫ ▫ ▫ ▫ ▫ ▫ Atheromatous emboli Strangulated hernias Immune complex disorders Trauma Segmental venous thrombosis Radiation therapy Oral contraceptives • Usually adequate collaterals to prevent infarction • Presentation: enteritis, stricture, acute abdomen ▫ Chronic can resemble Crohn's Focal Segmental Ischemia • Radiologic studies ▫ Smooth tapered stricture ▫ Abrupt change to normal distally ▫ Dilated proximally • Treatment: resection Colon Ischemia TYPE Reversible colopathy and transient colitis FREQUENCY (%)* >50 Transient colitis 10 Chronic ulcerating colitis 20 Stricture 10 Gangrene 15 Fulminant universal colitis <5 Colon Ischemia • Most common form of intestinal ischemia ▫ 7.2 cases per 100,000 person-years • Female predilection • Most > 60 years old • Young pt: vasculitis, coagulation disorders, cocaine, medications • Right colon ischemia ▫ May have small intestinal ischemia Medications • • • • • • • • • • • • • • • • Penicillins Alkaloid and taxanes Constipation-Inducing Agents Pseudoephedrine Diuretics Oral contraceptive pills Amphetamines (R sided) Cocaine (L sided) Kayexelate Magnesium citrate Sodium phosphate Bisacodyl Glycerin enemas NSAIDs Sumatriptan Alosetron Pathology • Mild: mucosal and submucosal hemorrhage and edema • More severe: ulcerations, crypt abscesses, pseudopolyps, pseudomembranes, iron-laden macrophages, submucosal fibrosis (stricture) • Most severe: transmural infarction Clinical Features • • • • • Sudden cramping Mild left lower quadrant pain Urgent desire to defecate Hematochezia within 24 hours Location: ▫ ▫ ▫ ▫ ▫ Sigmoid 23% Descending-to-sigmoid 11% Cecum-to-hepatic flexure 8% (worse prognosis) Descending 8% Pancolonic 7% Diagnosis • CT scan • If nonspecific, colonoscopy within 48 hours ▫ Unprepped, low air • Colon single-stripe sign ▫ Line of erythema with erosion or ulceration along the longitudinal axis of the colon ▫ Milder course Colonoscopy Treatment • NPO, IVF, antibiotics • EKG, Holter, echo • Colonic infarction ▫ Laparotomy and resection ▫ Serosa can be misleading • Segmental Ulcerating Colitis ▫ Recurrent fevers and sepsis ▫ Continuing or recurrent bloody diarrhea ▫ Persistent or chronic diarrhea with protein-losing colopathy ▫ Treat by resection Treatment • Ischemic Stricture ▫ Dilation or resection • Universal Fulminant Colitis ▫ Colectomy with ileostomy • Isolated Ischemia of the Right Colon ▫ Check CTA for concurrent AMI • Carcinoma/Obstructive Lesions (<5%) ▫ Lesion distal, increased intracolonic pressure proximal • Irritable Bowel Syndrome ▫ Colon ischemia 3.4 to 3.9x more common ▫ ?Hypersensitivity of the colonic vasculature • Complicating Aortic Surgery ▫ Up to 7% of surgeries (60% for ruptured aneurysm) ▫ Colonoscopy within 2-3 days if high risk Ex: ruptured aneurysm, prolonged cross-clamping time, post-op diarrhea Chronic Mesenteric Ischemia • “Intestinal angina” • Mesenteric atherosclerosis • Pain from small bowel ischemia ▫ Blood stolen to meet increased gastric demand from food Clinical Features • Gradual cramping discomfort within 30 minutes of eating, resolves over hours • Fear of eating, weight loss • Nonhealing antral ulcers without H. pylori • 1/3 to ½: cardiac, cerebral, peripheral vascular disease • Exam ▫ Abdomen soft and nontender ▫ Bruit common but nonspecific Diagnosis • Gastric tonometry exercise testing (GET) ▫ NG tube and arterial line ▫ Patient on PPI ▫ Obtain gastric juice and arterial blood fasting, during, after exercise ▫ Measure gastric-arterial PCO2 gradients ▫ Increase after exercise indicates ischemia • Combine with duplex U/S • Angiography ▫ Should show occlusion of ≥2 splanchnic arteries ▫ Does not make diagnosis in itself Treatment • Revascularization ▫ Need occlusive involvement of ≥2 major arteries ▫ Surgical if healthy ▫ Otherwise percutaneous +/- stent




![Paper_Prof_Wang_final1[1]](http://s3.studylib.net/store/data/005836194_1-85fb8d8882c087decd1a6d9c9fdc99c0-300x300.png)