Mesenteric Ischemia
advertisement

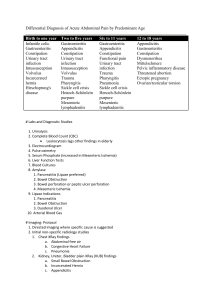
MedEd Portal Human Patient Simulation Title: Mesenteric Ischemia Target Audience: Emergency Medicine Resident Learning Objectives: - - - Environment: - - - Primary – Recognize mesenteric ischemia – Recognize that acute abdominal pain in elderly patients is associated with significant morbidity and mortality. Secondary – Recognize when the patient is decompensating and intervene with appropriate actions (IVF, blood, vasoconstrictive medications, consultation, antibiotics) Critical Actions Checklist – volume resuscitation – pain control – recognize atrial fibrillation on EKG – order abdominal CT as long as patient is stable – FAST if patient decompensates – antibiotics – type and cross – surgical consultation – consider anticoagulation but hold as patient is heme positive Environment – 25 bed ED in community hospital Manikin Set Up – Code cart – Intubation equipment – Code drugs – RSI drugs – Bedside ultrasound Props – EKG with atrial fibrillation with RVR – Negative FAST Distractors – Patient keeps asking for medicine during the history giving the resident a hard time obtaining information Actors: (All roles may be played by residents participating) Resident running the case Nurse to place IVs and give medications Another resident to be the Surgery or MICU consultant (able to give recommendations if necessary) Case Narrative: - Chief Complaint: Abdominal Pain - History: Seventy-seven year-old female presents with abdominal pain for the past 3 hours. It started soon after she finished eating lunch today. She saw her primary care doctor today who set her up for an outpatient abdominal ultrasound next week to evaluate her gallbladder. Her abdominal pain is generalized. She has had some loose stools, vomiting, and feels more short of breath lately. She states that she “just doesn’t feel good.” - Additional history given only if asked: There is history of “poor circulation” in her legs. Patient also notes that she’s lost 10 pounds without trying in the last 6 weeks and has occasionally had pain after eating. - PMHx: peptic ulcer disease, hypertension, hyperlipidemia - Social Hx: Retired schoolteacher who lives in a retirement community. - Meds: Hydrochlorothiazide; Simvastatin - Surgical Hx: Partial hysterectomy when she was 38 years old; carpal tunnel release surgery - Allergies: Penicillin - ROS: Subjective fevers and occasional chest discomfort - Physical Exam – BP 179/95, HR 111, RR 25, Temp 37.2, O2 sat 94%RA – GCS 15 in mild distress, clutching her abdomen – HEENT – NCAT, pupils 3mm bilaterally and reactive, EOMI – Resp – tachypnea; clear lungs bilaterally – CVS – tachycardia, irregularly irregular – Abd – soft, diffuse mild tenderness, a little more so in the epigastric region, no guarding or rebound, minimally diminished bowel sounds; no organomegaly – Rectal- moderate heme positive – – – Ext – no gross deformities; evidence of PVD in lower extremities bilaterally Neuro – completely intact Skin –pale, cool Instructors Notes: - Tips to Keep the Scenario Flowing – The patient should start out with relatively normal vital signs (except tachycardia) and progressively worsen throughout the simulation – Pain is not eased with IV opioids and the patient keep asking for more medication – Make sure the resident provides IV fluids and checks an EKG early on – Pain is initially out of proportion to exam. Over time, the patient’s abdomen becomes progressively more painful and peritonealemphasize the importance of serial abdominal exams - Tips to Direct Actors – The director should help the resident form a wide differential concerning her abdominal pain. - Scenario Steps – – – Optimal Management Path Resident realizes the many causes of abdominal pain in an elderly patient and forms a wide differential: gallbladder or liver etiology, pancreatitis, bowel obstruction, GI bleed/peptic ulcers, appendicitis, volvulus, mesenteric ischemia. The resident orders lab work including CBC, Chem 10, LFTs, lipase, amylase, and lactate. A 3 way abdominal film will be unremarkable. An abdominal CT should be ordered as well. An EKG and cardiac enzymes should be ordered based on her additional history of chest discomfort and shortness of breath. The EKG will pick up atrial fibrillation. This finding should clue the resident in to mesenteric ischemia. Surgery and intensivist consultations should be called. Potential Complications Path If the patient fails to recognize mesenteric ischemia in a timely manner, the patient decompensates and becomes septic quickly, requiring fluids, blood, and vasoconstrictive medications. Potential Errors Path - Topics to discuss – What is the classic triad of superior mesenteric artery embolism? – What is the definitive treatment for mesenteric ischemia? – What are the most common causes of mesenteric ischemia? – What are the pitfalls to diagnosing mesenteric ischemia? Pilot Testing and Revision: - Imaging and Labs – CBC: WBC 16, Hgb 11, Hct 32, Plts 214 – Chem 10: Na 135, K 3.6, Cl 101, CO3 22, BUN 12, Creat 1.3, Ca 8, Mg 2.1, Phos 4.3 – Lactate 2.1 – LFTs: AST 34, ALT 32, Alk Phos 121, Tbili 0.8 – Lipase 24 – Amylase 189 – D-dimer 301 – 3 way abdominal film: WNL – CT A/P: superior mesenteric artery ischemia – EKG: Atrial fibrillation with RVR Debriefing Plan: - The resident may not order an EKG and treat the atrial fibrillation with RVR which could progress into an unstable rhythm The resident may proceed with the GI bleed treatment pathway due to the heme positive stool Based on prior history of needing an ultrasound, the resident may order a RUQ ultrasound, delaying the definitive diagnosis. The relatively normal lactate may confuse the resident as to the diagnosis. (Initial lactate’s are not sensitive for mesenteric ischemia and should be repeated if persistent suspicion.) Number of Participants – 4 Evaluation form for participants – generic handout Authors: - John B. Seymour M.D. University of North Carolina Department of Emergency Medicine, PGY – 3 Rochelle Chijioke, M.D. University of North Carolina Department of Emergency Medicine, PGY-2 - Kevin Biese M.D. University of North Carolina Department of Emergency Medicine, Associate Professor and Residency Director Graham Snyder M.D. Wake Med Health and Hospitals Department of Emergency Medicine, Assistant Program Director and Simulation Director Jan Busby-Whitehead M.D. University of North Carolina Division of Geriatric Medicine/ Institute on Aging, Professor and Chief Copyright © 2011 The University of North Carolina School of Medicine