Dyspepsia
advertisement

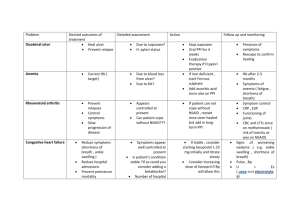
Dyspepsia, Peptic Ulcer Disease and Helicobacter Pylori Pharmacology & Therapeutics February 2007 Dyspepsia 40% of all adults 4% GP consultations 10% further investigations 10-20% NSAID users Endoscopy findings 15% Duodenal or Gastric ulcer 15% Oesophagitis = GORD 30% Gastritis duodenitis or hiatus hernia 30% Normal = functional dyspepsia Pathogenesis of Dyspepsia Factor Treatment approach Infection with H. pylori Eradication of H. pylori infection, e.g. triple tx ↑ gastric HCl secretion ↓ HCl secretion or neutralizing it, e.g. H2 antagonists, pirenzepine, antacids , PPIs Inadequate mucosal defence against gastric HCl Agents that protect gastric mucosa, e.g. sucralfate Altered gastric motility Prokinetic agents eg metoclopramide Gastric acid secretion Helicobacter Pylori Symptomatic treatment Antacids • MOA: Weak bases that react with gastric acid to form H20+salt. ↓pepsin activity as pepsin inactive at pH>4 • Symptom relief, liquids>tablets • E.g. Maalox = Mg(OH)2 + Al(OH)3 Drug Side effect Magnesium severe osmotic diarrhoea (therefore combined with AlOH) ↓ drug absorption Aluminium ↓phosphate, ↓absorption of tetracycline, thyroxine & chlorpromazine, constipation Calcium ↑Ca in blood & urine (high doses) Mucosal Protective Agents 1) Sulcralfate MOA: Binds to positively charged proteins present on damaged mucosa forming a protective coat Useful in “stress ulceration” As effective as H2-R antagonists/high dose antacids SE: Constipation ↓absorption of cimetidine, digoxin, phenytoin & tetracycline 2) Bismuth MOA: Antimicrobial action. Also inhibit pepsin activity, ↑mucus secretion & interact with proteins in necrotic mucosal tissue to coat & protect the ulcer crater Additional agents Antifoaming agent – Dimethicone to relieve flatulence (surfactant) Alginates - form a raft on surface of stomach contents to reduce reflux Carbenoxolone - liquorice derivative ? Alters mucin s/e H2O retention ↓K+ H2-receptor antagonists Drug Side effects Cimetidine -reversible impotence, gynaecomastia & ↓ sperm count (high doses) (nonsteroidal antiandrogen) -mental status abnormalities-confusion, hallucinations (elderly/renal impairment) -leukopenia & thrombocytopenia (rare) -cytochrome P450 inhibitor (e.g. impairs metabolism of warfarin, theophylline & phenytoin) Ranitidine,famotidine -Impotence, gynaecomastia & confusion less frequently than cimetidine. -Little interference with cytochrome P450 -Reversible drug-induced hepatitis with all H2antagonists Proton-pump Inhibitors (PPI) • MOA: block parietal cell H+/K+ ATPase enzyme system (proton pump) ↓ secretion of H+ ions into gastric lumen • More effective than H2-antagonists or antacids • Used in antimicrobial regimens to eradicate H. pylori • SE: n&v, diarrhoea, dizziness, headaches, gynaecomastia & impotence (rare), thrombocytopenia, rashes Helicobacter Pylori 95% Duodenal ulcers 70% Gastric ulcers 10% Non-ulcer dyspepsia Treatment benefits gastritis more than reflux symptoms Diagnosing H. pylori Urea breath test Stool antigen test Serology Endoscopy – CLO test 95% sensitive & specific 92% sensitive & specific 80% sensitive & specific 98% sensitive & specific (urea and phenol red, a dye that turns pink in a pH of 6.0 or greater) H. Pylori Eradication 1st line eradication tx for H. pylori 2nd line tx Preferred tx= PPI PO + Clarithromycin 500mg BD PO + Amoxicillin 1 gm BD PO for 7 days PPI + Bismuth 120mg QDS PO + Metronidazole 500mg TDS PO + Tetracycline 500mg QDS PO for 7 days If Penicillin allergic= PPI + Clarithromycin 500mg BD PO + Metronidazole 400mg BD PO for 7 days E.g. of PPI: Lansoprazole 30mg BD PO Subsequent failures handled on individual basis with advice from gastro/micro H. Pylori eradication 1 week triple-therapy regimens eradicate H. Pylori in >90% cases. Usually no need for continued antisecretory tx unless ulcer complicated by bleeding/perforation 2 week triple-therapy offer higher eradication rates cf 1 week but SE common & poor compliance 2-week dual-therapy with PPI & antibacterial produce low rates of H. pylori eradication & not recommended H. pylori eradication Treatment failure may be due to - Resistance to antibacterial drugs - Poor compliance Drug Side effects Bismuth n&v, unpleasant taste, darkening of tongue & stools, caution in renal disease Metronidazole n&v, unpleasant taste, ↓effectiveness OCP, care with lithium/warfarin Amoxicillin & tetracycline GI side effects, ↓ effectiveness OCP, pseudomenbranous colitis Lansoprazole ↓ effectiveness OCP Practical Management of dyspepsia Who needs endoscopy? GI bleeding Unintentional weight loss Dysphagia Persistent vomiting Iron deficiency anaemia Epigastric mass >55 with unexplained persistent/recent onset dyspepsia PUD on endoscopy Stop NSAIDs Start full dose PPI for 2 months Eradication treatment if H Pylori positive Repeat endoscopy for gastric ulcer 2% cancer risk GORD on endoscopy Lifestyle advice Full dose PPI for 1-2 months H Pylori Eradication may not benefit reflux symptoms If recurrence - lowest dose PPI to control symptoms GORD GORD = Symptoms of “heartburn” General advice includes AVOIDING Drug Tx Meals antacids=+/-alginic at night, lying down after meals Elevate head of bed Heavy lifting, tight clothing, bending Being overweight Smoking (nicotine relaxes lower oesophageal sphincter) Aggravating substances (spicy foods, C2H5OH) Drugs which encourage reflux (e.g. antimuscarinic, smooth muscle relaxants, theophylline) acid Pro-kinetic agent, e.g. metoclopramide H2-antagonist PPI If severe sx when tx stopped, or bleed from oesophagitis or stricture maintenance tx with PPI or surgery may be necessary NSAID Induced Dyspepsia 10-20% develop endoscopically visible PUD 1-5% perforation or major bleeding Endogenous prostaglandins (PGE2 & I2) contribute to GI mucosa integrity by - stimulation of mucus & bicarbonate secretion - maintenance of blood flow (allows removal of luminal H-ions) - prevent luminal H-ions from diffusing into the mucosa - ↓ gastric acid secretion - helping to repair damaged epithelium NSAID Induced Dyspepsia Elderly >65 years History PUD Other drugs – eg bisphosphonates, Steroids PPI or misoprostol protection for at risk Consider screening & eradicating H Pylori infection Prostaglandin analogues • Misoprostol = synthetic prostaglandin E1 analogue Prevents NSAID induced ulcers & heals chronic GU & DU SE: Abdo pain, n&v, diarrhoea, abortifacient (produces uterine contractions) Non ulcer dyspepsia Treat H pylori (no routine retesting) Symptomatic treatment PPI (proven benefit) Prokinetic agent eg metoclopramide (probable benefit) Dyspepsia without alarm symptoms Lifestyle advice Antacids and medication review Empiric PPI Test and treat for H Pylori Shah, R. BMJ 2007;334:41-43 Copyright ©2007 BMJ Publishing Group Ltd.