GERD Ambulatory Mini-Lecture
advertisement

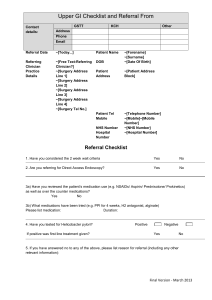
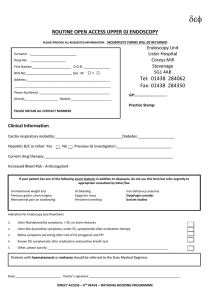
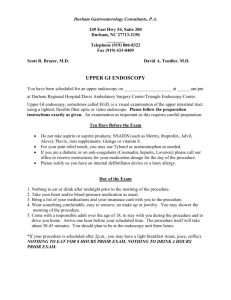
GERD Ambulatory Mini-Lecture Gastro-Esophageal Reflux Disease • The condition of chronic, pathologic reflux of acidic stomach contents – Esophagus – Oropharynx – Larynx, even lungs • Leads to symptoms and/or mucosal damage – NERD = symptoms without damage – Symptoms may be typical or atypical Typical Symptoms • Heartburn – – – – – Retrosternal burning sensation Most commonly post-prandial, nocturnal Fatty foods, spicy foods, acidic foods Relived with antacids, water, milk Worsened with recumbency • Acid Regurgitation – Perception of gastric content reflux in the mouth or hypopharynx – AKA water brash: bitter, acidic Atypical Symptoms • Atypical – – – – Dysphagia, odynophagia Nausea Chest pain Dyspepsia = non-severe upper abdominal discomfort • Epigastric fullness, bloating • Frequent belching • Heartburn • Extraesophageal – – – – Chronic cough Hoarseness, laryngitis Vocal Cord Dysfunction, Bronchospasm Globus sensation Complications of GERD • • • • • Peptic stricture Metaplastic disease (Barrett’s) Dysplastic disease (adenocarcinoma) Laryngitis Pulmonary disease Red Flags…think endoscopy • • • • • • • Dysphagia/odynophagia Nausea/vomiting Melena, anemia* Weight loss, anorexia Extended duration of symptoms No response to PPI Family history of PUD • Caucasian Male, 50+ years old, sx > 10 yrs – Concern for Barrett esophagitis Diagnosis • • • • History Trial of PPI Upper Endoscopy Esophageal pH monitoring • Presumptive GERD diagnosis can be based on clinical symptoms alone and can start with empiric therapy Diagnostic Considerations • Esophagitis – Infectious: Fungal vs viral – Pill – Eosinophilic (Allergic) • H. pylori testing prior to PPI • CAD – Women – Elderly – Diabetics Work up • History + Empiric treatment – Although a response to PPIs is not a definitive diagnosis of GERD, in clinical practice it is more appropriate to start empiric treatment than to pursue reflux pH monitoring – Symptoms that do not improve warrant further evaluation to demonstrate the existence of GERD and evaluate for an alternate diagnosis Endoscopy with biopsy • Upper endoscopy is not required for diagnosis • Indicated for suspected GERD plus – Red flags, or – Symptoms resistant to twice daily PPI therapy • Esophagitis or Barrett’s esophagus = diagnostic • Remember NERD – 62% of patients with typical symptoms of GERD will have a normal EGD Other diagnostic work up • Ambulatory pH monitoring – Persistent symptoms despite medical therapy – Confirmatory testing in patients with normal EGD • No Barium • Esophageal manometry for dysmotility Articles • Badillo R, Francis D. Diagnosis and treatment of gastroesophageal reflux disease. World Journal of Gastrointestinal Pharmacology and Therapeutics 2014; 5(3):105-112. doi: 10.4292/wjgpt.v5.i3.105. • Achem SR, DeVault KR. Gastroesophageal reflux disease and the elderly. Gastroenterol Clin North Am. 2014 Mar; 43(1):147-60. doi: 10.1016/j.gtc.2013.11.004. Review. PubMed PMID: 24503365 • Vela MF. Medical treatments of GERD: the old and new. Gastroenterol Clin North Am. 2014 Mar; 43(1):121-33. doi: 10.1016/j.gtc.2013.12.001. Epub 2013 Dec 31. Review. PubMed PMID: 24503363 • Overland MK. Dyspepsia. Med Clin North Am. 2014 May; 98(3):54964. doi: 10.1016/j.mcna.2014.01.007. Epub 2014 Mar 18. Review. PubMed PMID: 24758960 MKSAP QUESTIONS Question 1 A 35 yo woman is evaluated for a 6 month history of an upset stomach that usually occurs after meals. She also has heartburn symptoms after meals at least 4 times per week. She reports no difficulty of pain with swallowing an no vomiting, weight loss, altered stool habits or blood in the stool. There is no family history of malignancy. On physical examination, the vital signs are normal. Abdominal examination discloses a non-tender epigastrium and no masses or lymphadenopathy. CBC is normal. Question 1 Which of the following is the most appropriate management? A. Proton pump inhibitor B. Sucralfate C. Test for Helicobacter pylori and treat if positive D. Upper endoscopy Question 1 Explanation Educational Objective Manage dyspepsia and heartburn with proton pump inhibitor therapy. The best first line treatment for this patient is acid suppression with a proton pump inhibitor (PPI). This patient is considered to have GERD with dyspeptic features. Studies have shown that patients with dyspepsia who undergo endoscopy commonly have normal findings. However, the most common finding in patients with abnormalities is esophagitis. PPI is thought to be superior to H2 blockers for both dyspepsia and heartburn. Sucralfate does not have a role in the treatment of GERD and has no advantage when compared with placebo for treatment of functional dyspepsia. A test-and-treat strategy for H. pylori would be appropriate for patients with dyspeptic symptoms without heartburn or alarm symptoms and who are fun an area with high prevalence of H. pylori infection (>20%). Because this patient also has heartburn, this approach is incorrect. There has been some controversy as to whether eradication of H. pylori in patients with dyspepsia may increase the risk of post-eradication GERD, but a recent meta analysis has shown this to be true. An upper endoscopy is incorrect because this patient does not have alarm symptoms such as onset after the age of 50, anemia, dysphagia, odynophagia, vomiting, weight loss, family history of upper GI malignancy, personal history of peptic ulcer disease, gastric surgery or GI malignancy, and abdominal mass or lymphadenopathy on examination. Question 2 A 40 year old woman is evaluated for a 1 year history of reflux symptoms. She has heartburn and regurgitation of gastric contents several times a week. She was placed on lifestyle modifications and an empiric trial of a once daily proton pump inhibitor (PPI) 12 weeks ago with minimal relief of symptoms. For the past 6 weeks, se has taken the PPI twice daily, with minimal relief. She has had intermittent solid food dysphagia. She appears to be adherent to her lifestyle and medical therapy. Physical examination discloses normal vital signs and a BMI of 35. Question 2 Which of the following is the most appropriate next step in management? A. Add an H2 blocker at night B. Ambulatory esophageal pH study C. Endoscopy D. Fundoplication Question 2 Explanation Educational Objective Manage GERD that does not respond to an empiric trial of PPI therapy This patient should undergo endoscopy. Her symptoms suggest GERD and there has been no response to empiric trials of high dose PPI for an adequate period of time (8-12 weeks). Further evaluation with endoscopy is required for patients with symptoms of weight loss, dysphagia, odynophagia, bleeding or anemia and in men with long standing symptoms (>5 years) or symptoms that are refractory to acid suppression therapy. This patient has had intermittent dysphagia to solid food and her symptoms appear to be refractory to PPI therapy; she should therefore undergo endoscopy to explore complications and alternative diagnoses such as eosinophilic esophagitis, stricture, malignancy or achalasia. PPIs are much more effective in healing esophagitis compared to H2 blockers. Adding H2 blockers to maximal PPI therapy does not result in a meaningful increase in acid blockade. Therefore, an additional dose of an H2 blocker is unlikely to produce relief for patients who continue to have heartburn after 6 weeks of treatment with a PPI. Ambulatory esophageal pH monitoring is most commonly used to confirm GERD in patients with persistent symptoms despite maximal medical therapy and an unrevealing endoscopy. In this patient with persistent symptoms and intermittent dysphagia, endoscopy is the most appropriate next diagnostic test to assess for evidence of reflux induced complications. If endoscopy is unrevealing, ambulatory pH monitoring should be considered. Persistent or recurrent symptoms despite maximal medical therapy for GERD are indications for anti-reflux surgery such as fundoplication. However, before consideration of anti-reflux surgery, this patient should undergo endoscopy to confirm the presence of esophagitis and to eliminate the possibility of another diagnosis and possibly ambulation pH recording. Question 3 A 75 year old man is evaluated in follow up after recent surveillance endoscopy for Barrett esophagus. Biopsy from one of the salmon colored columnar segment shows high grade dysplasia. His GERD symptoms are well controlled with proton pump inhibitor therapy. His medical history is significant for New York Heart Association functional class III heart failure (Ejection fracture of 30%). His medications are pantoprazole, furosemide, digoxin, metoprolol, enalapril and spironolactone. On physical examination, he is afebrile, blood pressure is 100/50 mmHg, pulse rate is 62/min, and respiratory rate is 12/min. BMI is 35. There is no evidence of jugular venous distention. Cardiac rhythm is regular with a soft S3 at the cardiac apex. The lungs are clear. No peripheral edema is present. Question 3 Which of the following is the most appropriate management? A. Endoscopic ablation B. Esophagectomy C. Fundoplication D. Repeat endoscopic surveillance in 3 years Question 3 Explanation Educational Objective Manage high grade dysplasia in a patient with Barrett esophagus. This patient should receive endoscopic ablation. Options for the management of high grade dysplasia in patients with Barrett esophagus include esophagectomy, and endoscopic therapy (combined mucosal resection and ablation of residual BE). However, esophagectomy is associated with a mortality rate of 2-8% and a morbidity rate of 30-40% in the immediate postoperative period. This patient has a significant medical comorbid condition and is a suboptimal candidate for esophagectomy. Endoscopic therapy is a reasonable alternative because of its lower morbidity rates, especially in patients with high surgical risk. Results of endoscopic therapy have been shown in cohort studies to be comparable with those of esophagectomy. Fundoplication is recommended when uncontrolled GERD symptoms persist despite maximal medical therapy; however, this patients symptoms are well controlled with PPI. Fundoplication has not been shown to reduce the risk of BE progression to dysplasia or cancer compared with medical therapy. Repeat endoscopic evaluation would be recommended at intervals of no longer than 3 months because of ht4e substantial risk of progression of high grade dysplasia to adenocarcinoma (6% per year) and risk of coexisting neoplasia (1012%). If subsequent surveillance detects progression to adenocarcinoma, endoscopic therapy can be utilized at that time. Question 4 A 44 year old woman is evaluated for a 1 year history of vague upper abdominal discomfort that occurs after eating. She is from a rural area in a developing country. She has not had nausea, vomiting, dysphagia, odynophagia, weight loss or black or bloody stools. She is otherwise healthy. She has no personal history of peptic ulcer disease and no family history of gastrointestinal malignancy. Her only medication is a multivitamin. On physical examination, temperature of 36.8C/98.2F, blood pressure is 127/82 mmHg, pulse rate is 72/min, and respiration rate is 16/min. BMI is 27. There is epigastric tenderness with moderate palpitation but no masses or lymphadenopathy. Complete blood count is normal. Question 4 Which of the following is the most appropriate management? A. Helicobacter pylori stool antigen testing B. Initiate an H2 blocker C. Initiate empiric treatment for H. pylori infection D. Perform endoscopy Question 4 Explanation Educational Objective – Manage dyspepsia without alarm feature in a patient from a developing country The most appropriate management for this patient is stool antigen testing for Helicobacter pylori. Dyspepsia is chronic or recurrent discomfort in the upper mid-abdomen. The prevalence of dyspepsia is not well known because of the vagueness of its description by both patients and physicians. In addition to discomfort, affected patients may have mild nausea or bloating. The recommended approach for a patient younger than 50 years without alarm features (anemia, dysphagia, odynophagia, vomiting, weight loss, family history of upper GI malignancy, personal history of peptic ulcer disease, gastric surgery or gastrointestinal malignancy and abdominal mass or lymphadenopathy on examination) is a test an treat strategy for H. pylori or empiric treatment with a proton pump inhibitor. The test and treat strategy for H. pylori is an appropriate first line a strategy when the patient is from an area where prevalence of H. pylori is high (such as developing countries); however, PPI is the most appropriate first line strategy if the patient is from an area where prevalence of H. pylori is low. Pats such as this one from developing countries have a high prevalence of H. pylori owing to likely fecal oral transmission. Therefore, for this patient, a test and treat approach is preferred. If testing is positive, eradication of H. pylori may relieve symptoms, but it is important to note that randomized controlled trials provide conflicting results as to the efficacy of H. pylori eradication in improving symptoms of functional dyspepsia. If the patient does not test positive for H. pylori, a trial of PPI is warranted. PPIs are superior to H2 blockers, so initiating an H2 blocker would not be appropriate in this patient. Empiric treatment for H. pylori is incorrect because the diagnosis of H. pylori should be determined before initiating treatment. Endoscopy would be appropriate for patients who symptoms do not respond to H. pylori treatment or PPI therapy. Patients older than 50 years or with alarm feats should always be evaluated with upper endoscopy. In patients without alarm features , endoscopy as an initial management intervention would be unlikely to find gastritis, peptic ulcer disease, or esophagitis.