Dyspepsia - CCRMC Wiki
advertisement

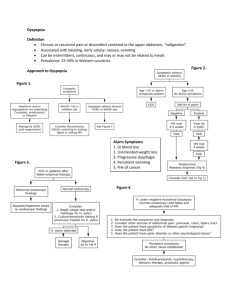
Dyspepsia Neil C. Jackson General Common symptom with extensive differential diagnosis and heterogenous pathophysiology. Epidemiology 25% of general population/year 25% with evidence of organic cause 75% without Symptoms Chronic or recurrent pain or discomfort in the upper abdomen Ulcer-like or acid dyspepsia Burning pain, epigastric huger-like pain Relief with food/antacids/antisecretory agents Food-provoked dyspepsia or indigestion Postprandial epigastric discomfort and fullness Belching, early satiety, nausea, occasional vomiting Reflux-like dyspepsia Rome III Criteria Postprandial fullness Early satiation Inability to finish a normal sized meal Epigastric Pain or Burning Organic dyspepsia PUD GERD GE malignancy Biliary Meds (NSAIDs) Other Celiac / chronic pancreatitis Infiltrative dz (Eosinophilic gastritis / crohn’s / sarcoid) DM radiculopathy / hypercalcemia / heavy metal toxicity Hepatoma / steatohepatitis / mesenteric ischemia PUD A spectrum from gastritis to ulceration complicated by bleeding, pain and perforation. Poor correlation with reported symptoms and EGD findings Includes Duodenal and gastric ulcers Commonly due to H.Pylori and/or NSAID, tobacco, EtOH Treatment = H.pylori eradication and removal of inciting agents Duodenal vs. Gastric Ulcers Gastric ulcer Worse with meals Poor response to antacids/otcs Duodenal ulcer Pain when acid is secreted in absence of a food buffer Improves with meals, alkali, antisecretory agents Worse 3-5 hours after a meal Worse at night between 11pm – 2am Maximal circadian stimulation of acid secretion GERD Some degree of reflux is physiologic Montreal classification: A condition that develops when reflux of stomach contents causes troublesome symptoms and/or complications Prevalence= 10-20% in western world, <5% in Asia Heartburn = retrosternal burning, most common Regurgitation = gastric content into mouth/throat Dysphagia = common in longstanding GERD due to Reflux esophagitis Stricture More GERD Globus sensation Almost constant perception of a lump in the throat Water brash (foaming at the mouth) Rare hypersalivation caused by reflux Chest pain Mimics angina, typically squeezing/burning Substernally with radiation to back/neck/jaw/arms Lasts minutes to hours Spontaneous resolution with antacids Occurs after meals, awakens from sleep Worse with emotional stress GE Malignancy Uncommon cause of chronic dyspepsia in Western Hemisphere More common in Asian, Hispanic, Afro-Caribbean populations Increases with age Epigastric pain vague, mild in early disease – more severe and constant with progression Weight loss from insufficient caloric intake Dysphagia related to esophageal or proximal gastric malignancy NSAIDs Direct effect Ionization upon absorption into gastric mucosa Topical epithelial injury Systemic effect Inhibition of GI mucosal COX activity (COX1) Decreased mucosal prostaglandin protection History Association of symptoms with meals Heartburn / regurgitation / cough NSAID use ?? Radiation to back, personal/fhx of pancreatitis Significant weight loss / anorexia / vomiting / dysphagia / odynophagia / fhx of GI malignancy Severe episodic epigastric / RUQ pain lasting more than one hour Exam Usually normal except for epigastric tenderness Jaundice, pallor, ascites, muscle wasting Palpable abdominal mass Palpable lymphadenopathy L supraclavicular = Virchow’s node Periumbilical = Sister Mary Joseph’s node Carnett sign Double straight leg raise or head raise while supine Finger presses point of tenderness + test = Increased pain with muscle tensing Labs CBC Electrolytes + Calcium Hepatic Function Panel Alarm Features Age > 55 yrs with new-onset dyspepsia FHx of upper GI malignancy Unintended weight loss GI bleeding Progressive dysphagia Odynophagia (painful swallowing) Unexplained Iron deficiency Persistent vomiting Palpable mass or node Jaundice Diagnosis: Pt with alarm features Upper endoscopy within two weeks with stomach biopsy for H.pylori Yield of EGD increases with age Per meta-analysis of 9 studies, 5389 pts: 6% erosive esophagitis 8% PUD If normal, most will have functional dyspepsia Further evaluation warranted if alarm features Age cutoff controversial AGA suggests 60-65 yrs 45-50 with Asian, Hispanic, Afro-Caribbean descent Reflux Esophagitis Barrett’s Esophagus Gastric Ulcer Esophageal Ulcer Diagnosis: No alarm features Test and treat for H.pylori If local h.pylori prevalence >10 % Empiric PPI / H2blocker If local h.pylori presence <5% Test and Treat for H.Pylori Urea breath test or stool Ag Serologic testing should not be used NNT is 14 H. Pylori eradication Quadruple Therapy Triple therapy + bismuth 525mg 4xdaily for 10-14 days With clarithromycin/metronidazole resistance > 15% With recent/repeated exposure to clarithro/flagyl Triple Therapy PPI (multiple options) Omeprazole 20mg bid Pantoprazole 40mg bid Amoxicillin: 1g BID 7-14 days Clarithromycin: 500mg BID 7-14 days Alternative antibiotics Doxycycline 100mg bid / Flagyl 250mg 4xdaily Anti-Secretory Therapy PPIs > H2 blockers PPI (Omeprazole / pantoprazole / lansoprazole ) Irreversibly binds/inhibits H/K atp pump on parietal cells Only effective in active parietal cells Must be taken 30-60 minutes before meals Twice daily dosing if : Failed standard therapy Large gastric ulcer H2 blockers (Ranitidine / cimetidine / famotidine) Inhibit Histamine H2 receptors on parietal cells Functional Dyspepsia Presence of one or more: Postprandial fullness Early satiation Epigastric pain/burning Negative diagnostic evaluation for organic disease Symptoms for last three months Onset more than 6 months previously Pathophysiology Gastric motility / compliance Delayed gastric emptying (30%) rapid gastric emptying (10%) Visceral hypersensitivity Increased pain with normal gastric stretching/compliance Independent of delayed gastric emptying H.pylori infection Unclear mechanism, ?smooth muscle dysfunction 2/2 inflammatory modulation of enteric nervous system Altered gut microbiome Symptoms more likely after episode of AGE Psychosocial dysfunction Association with GAD, somatization, Major Depression Higher prevalence in pts with self-reported hx of child abuse Treatment H.Pylori test and treat Tricyclic anti-depressants If persistent symptoms despite PPI x8wks PPI / H2 blockers Metoclopramide (Prokinetic) If failed above therapy 5-10 mg TID half hour before meals and at night x4wks References Uptodate Approach to the Adult with Dyspepsia Functional dyspepsia in adults Clinical manifestations of peptic ulcer disease Clinical manifestations and diagnosis of GERD in adults Clinical features,diagnosis,staging of gastric cancer Epidemiology, pathobiology and clinical manifestations of esophageal cancer Differential diagnosis of abdominal pain in adults AGA AGA medical position statement: evaluation of dyspepsia – Gastroenterology, 2005 AFP Evaluation and management of non-ulcer dyspepsia H.Pylori Infection