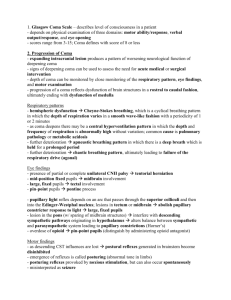
COMA
advertisement

COMA DR RABIA RATHORE ASSISTANT PROFESSOR WEST MEDICAL WARD MAYO HOSPITAL/K.E.M.U COMA DR RABIA RATHORE ASSISTANT PROFESSOR WEST MEDICAL WARD MAYO HOSPITAL/K.E.M.U DEFINITION OF COMA A state of prolonged unconsciousness characterized by loss of reaction to external stimuli or, a state of unarousable unresponsiveness. Consciousness is dependent on the functioning of two separate anatomical and physiological systems: The ascending reticular activating system (ARAS) projecting from brainstem to thalamus. This determines arousal (the level of consciousness) The cerebral cortex, which determines the content of consciousness. Impaired functioning of either anatomical system may cause coma. FEATURES DISTINGUISHING BETWEEN COMA AND RELATED STATES STUPOR Unconscious but can be aroused with repeated stimuli.. DELIRIUM : Confused state often with restlessness and hallucinations . ‘LOCKED-IN SYNDROME : Actually conscious but unable to speak or move may move eyes (massive brainstem damage). Awarness is present , sleep awake cycles are present, vertical eye movement /blinking may be seen. Respiration is preserved. VEGETATIVE STATE : Apparently awake but unresponsive (brainstem intact but widespread cortical damage). Awarness is absent ,while sleep awake cycles are present. There is no purpose movement ,respiration is preserved . ― COMA: The Awarness is absent, sleep awake cycles are absent.There is no purposeful movement and respiration is variable.. BRAIN DEATH : There is lack of awarness, sleep awake cycles are absent.There is no purposeful movement ,respiration is absent CAUSES OF COMA DIFFUSE BRAIN DYSFUNCTION: Drug overdose (accidental or deliberate), including alcohol CO poisoning Traumatic brain injury Hypoglycaemia, hyperglycaemia Severe uraemia Hepatic encephalopathy Respiratory failure with CO2 retention Hypercalcaemia, hypocalcaemia Hypoadrenalism, hypopituitarism and hypothyroidism Hyponatraemia, hypernatraemia Metabolic acidosis Hypothermia, hyperpyrexia Seizures – post-ictal state and non-convulsive status Metabolic rarities, e.g. porphyria Extensive cortical damage Hypoxic-ischaemic brain injury, e.g. cardiac arrest Encephalitis, meningitis, cerebral malaria Subarachnoid haemorrhage DIRECT EFFECT WITHIN BRAIN STEM: Brainstem haemorrhage, infarction or demyelination Brainstem neoplasm, e.g. glioma Wernicke–Korsakoff syndrome PRESSURE EFFECT ON BRAIN STEM: Tumour, massive hemisphere infarction with oedema, haematoma, abscess Cerebellar mass IMMEDIATE ASSESMENT OF COMATOSE PATIENT Check the airway, breathing and circulation. Check for blood glucose. Obtain as much history as possible. What were the circumstances? Ask paramedics, police, and witnesses. Contact the patient’s relatives, friends and GP and obtain past hospital notes. Look for drug details/bottles and identification data. GENERAL EXAMINATION Measure the patient’s temperature.Check for meningism. Sniff the patient’s breath for ketones, alcohol and hepatic fetor. Survey the skin for signs of trauma or spinal injury, rash (meningococcal sepsis), jaundice or stigmata of chronic liver disease, cyanosis, injection marks. Respiratory pattern: Cheyne–Stokes (alternating hyperpnoea and periods of apnoea indicating bilateral cerebral or upper brainstem dysfunction) Acidotic (Kussmaul) respiration (deep, sighing hyperventilation seen in diabetic ketoacidosis and uraemia). NEUROLOGICAL EXAMINATION Neurological examination aims to determine: Depth of coma (GCS) Brainstem function Lateralization of pathology BRAIN STEM FUNCTION PUPILS: Record their size and reaction to light Dilatation of one pupil that then becomes fixed to light Compression of the IIIrd nerve. Bilateral mid-point reactive pupils (i.e. normal pupils) Metabolic comas Sedative drugs except opiates. Bilateral light-fixed, dilated pupils: Brain death. Barbiturate intoxication hypothermia. Bilateral pinpoint, light-fixed pupils: Pontine haemorrhage Opiates. Mydriatic drugs previous pupillary surgery LATERALIZING SIGNS Coma makes it difficult to recognize lateralizing signs. These are helpful: Asymmetry of response to visual threat in a stuporose patient: suggests hemianopia Asymmetry of face. Drooping or dribbling on one side, blowing in and out of mouth when the paralysed cheek does not move Asymmetry of tone. Unilateral flaccidity or spasticity may be the only sign of hemiparesis Asymmetry of decerebrate and decorticate posturing Asymmetrical response to painful stimuli Asymmetry of tendon reflexes and plantar responses. Both plantars are often extensor in deep coma. CLINICAL PRESENTATION CASE SCENARIO NO:1 A young college boy had high grade fever for 3 days. Fever was associated with photophobia.Now for the last 5 hours he developed sudden severe headache all around the head, 2 episodes of vomiting which were projectile in nature followed by altered state of consciousness.His examination revealed a young male who was unconscious with pulse of 55 beats per minute ,blood pressure 160/90, signs of meningeal irritation were present. What is the differential diagnosis? Acute Bacterial Meningitis Subarachnoid haemorrhage Migraine CAUSES OF MENINGITIS Bacteria Neisseria meningitidis Streptococcus pneumoniaea Staphylococcus aureus Streptococcus Group B Listeria monocytogenes Gram-negative bacilli, e.g. E. coli Mycobacterium tuberculosis Treponema pallidum • Viruses • Epstein–Barr virus • Enteroviruses • Coxsackie virus • Poliomyelitis • Mumps • Herpes simplex • HIV Fungi Cryptococcus neoformans Candida albicans Coccidioides immitis, Histoplasma capsulatum, Blastomyces dermatitidis (USA) CLINICAL CLUES IN MENINGITIS Clinical feature Petechial rash Skull fracture Ear disease Congenital CNS lesion Immunocompromised patients Rash or pleuritic pain International travel Occupational (work in drains, canals, polluted water, recreational swimming) Possible cause : Meningococcal infection Pneumococcal infection HIV opportunistic infection Enterovirus infection Malaria Leptospirosis CLINICAL FEATURES MENINGOCOCCAL RASH How will you investigate him? INVESTIGATIONS Blood complete examination & ESR Blood cultures CT scan Lumbar puncture CSF PICTURE COMPLICATIONS OF MENINGITIS ACUTE COMPLICATIONS: Seizures cranial nerve lesions venous sinus thrombosis severe cerebral oedema hydrocephalus CHRONIC COPMLICATIONS: Focal neurological Behaviour disorder Language deficit Deafness Seizure disorder CASE SCENARIO NO 2 An old retired army officer who is diabetic and hypertensive with poor compliance of medicine developed severe headache and two episodes of vomiting, just after the last episode of vomiting he fell down to the ground ,developed altered state of consciousness and was brought to emergency by his son . On examination GCS was 3/15 there were pin point pupil ,horizontal eye movements of eyes were absent while vertical eye movements were present . His BP was 230/140mm of Hg and temperature was 104*F. Respiratory rate was 32/min and was having qudreplegia. What is the diagnosis? PONTINE HEMORRHAGE How will you investigate him? The purpose of investigations in stroke is: To confirm the clinical diagnosis and distinguish between haemorrhage and thromboembolic infarction; To look for underlying causes and to direct therapy; To exclude other causes, e.g. tumour. Sources of embolus should be sought. Routine bloods (for ESR, polycythaemia, infection, vasculitis, thrombophilia, syphilitic serology, clotting studies, autoantibodies) Fasting Lipid profile Chest X-ray ECG E chocardiography Carotid Doppler studies MR angiography PT/APTT Bleeding time/Clotting time Imaging in Acute Stroke. Non-contrast CT: will demonstrate haemorrhage immediately but cerebral infarction is often not detected or only subtle changes are seen initially. CT SCAN BRAIN MR angiography showing internal carotid artery occlusion. DEFINITION Stroke Stroke is defined as a syndrome of rapid onset of cerebral deficit (usually focal) lasting >24 h or leading to death, with no cause apparent other than a vascular one. Transient ischaemic attack (TIA) means a brief episode of neurological dysfunction due to temporary focal cerebral or retinal ischaemia without infarction. TIAs may herald a stroke Risk factor for Ischemic stroke : Hypertension Diabetes Smoking Lifestyle High cholesterol Atrial fibrillation Obesity Severe carotid stenosis RARE CAUSES: Hyperviscosity states. Thrombocythaemia, Polycythaemia Thrombophilia Anti-cardiolipin and lupus anticoagulant antibodies oral contraceptive. Migraine Vasculitis Systemic lupus erythematosus (SLE), Polyarteritis Giant cell arteritis . granulomatous CNS angiitis Amyloidosis. Hyperhomocysteinaemia Neurosyphilis mitochondrial disease Drugs : Sympathomimetic drugs cocaine Vasoconstrictors neuroleptics CADASIL (cerebral dominant arteriopathy with subcortical infarcts and leucoencephalopathy) WHAT IS THE LESION ? WHERE IS THE LESION ? CASE SCENARIO An 18 years old girl is brought to emergency in unconscious state .Her mother gave a history that she was havimg polyuria and polydipsia for the last few months.2 days back she complained of abdominal pain which worsened gradually,7-8 episodes of vomiting and now has developed altered state of consciousness which was gradual in onset.On examinationshe was in a stuporous state with evidence of dehydration, rapid deep breathing with “fruity” breath odor of acetone .Her pulse was 110 bpm and BP.60/40 mm of Hg. What is the diagnosis? DIABETIC KETO ACIDOSIS HOW ARE U GOING TO INVESTIGATE HER? INVESTIGATIONS BLOOD COMPLETE EXAMINATION BLOOD SUGAR LEVEL URINE FOR KETONES/COMPLETE EXAMINATION SERUM KETONES SERUM ELECTROLYTES SERUM OSMOLALITY mosm/kg =Measured[Na ]+Glucose (mg/dL) 18 Blood urea nitrogen Serum creatinine Arterial blood gases TERMS USED IN UNCONTROLLED DIABETES Ketonuria Detectable ketone levels in the urine; it should be appreciated that ketonuria occurs in fasted non-diabetics. Ketosis Elevated plasma ketone levels in the absence of acidosis Diabetic ketoacidosis Hyperosmolar Hyperglycaemic state A metabolic emergency in which hyperglycaemia is associated with a metabolic acidosis due to greatly raised (>5 mmol/L) ketone levels. A metabolic emergency in which uncontrolled hyperglycaemia induces a hyperosmolar state in the absence of significant ketosis Lactic acidosis A metabolic emergency in which elevated lactic acid levels induce a metabolic acidosis and associated with biguanide therapy CASE SCENARIO NO:3 A middle aged female had a history of slowness in her activities, dry brittle hairs and thick-skin.She also complains of deep-voice with weight gain, cold intolerance and constipation.There is also history of oligomenorrhoea.Now has presented in emergency in semi conscious state.On examination she had puffy eyes ,loss of lateral 1/3of eye brows,peripheral non pitting edema .Her pulse was 55 bpm.Heart sounds were muffled.Her temperature was below normal. What is the diagnosis? Myxoedema coma CASE SCENARIO NO:3 A young female was brought in emergency when she was found unconscious in room by his husband.Past history revealed that she has been on treatment for depression since 4-5 months after the death of her son.On further inquiring her husband it was found that she had a fight with her husband on some minor issue one day back .Examination revealed that she had dilated pupils, dry mouth, flushed skin and muscle twitching.Her pulse was 120/minute and she was in deep coma. What is the diagnosis? TRICYCLIC ANTIDEPRESSANT POISONING MANAGEMENT Cardio toxic sodium channel-depressant effects of tricyclic antidepressants may respond to boluses of sodium bicarbonate (50–100 mEq intravenously). Prolongation of the QT interval or torsades de pointes is usually treated with intravenous magnesium. Severe cardio toxicity in patients with overdoses has responded to intravenous lipid emulsion. Plasma exchange using albumin has been reported to b successful in few cases. Mild serotonin syndrome may be treated with benzodiazepines. Moderate cases may respond to cyproheptadine (4 mg) orally or via gastric tube hourly for three or four doses) or chlorpromazine (25 mg intravenously). Severe hyperthermia should be treated with neuromuscular paralysis and endotracheal intubation in addition to external cooling measures.