COMA and Acute Confusional States - asja
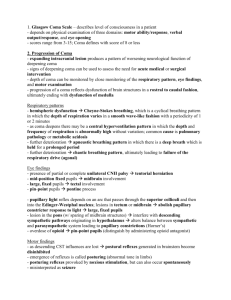
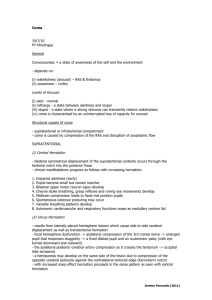
advertisement
Prof., Dr. :sherif wadie Reticular activating system (RAS) Good Consciousness = Alertness + Awareness Diminished alertness = Widespread abnormalities of cerebral hemispheres or reduced activity of reticular activating system (RAS) Confusion : Impaired attention and concentration, manifest disorientation in time, place and person, impersistent thinking, speech and performance, reduced comprehension and capacity to reason Fluctuate in severity, typically worse at night ‘sundowning’ Perceptual disturbances and misinterpret voices, common objects and actions of other persons Confusion is also found in dementia (progressive failure of language, memory, and other intellectual functions) Delirium : confusion and associated agitation, hallucination, convulsion and tremor Amnesia : a loss of past memories and to an ability to form new ones, despite alert and normal attentiveness Alert : normal awake and responsive state Drowsiness : state of apparent sleep, briefly arousal with oral command Lethargic : resembles sleepiness, but not becoming fully alert, slow verbal response and inattentive. Unable to adequately perform simple concentration task (such as counting 20 to 1) Somnolent : easily aroused by voice or touch; awakens and follows commands; required stimulation to maintain arousal Obtunded/Stuporous : arousable only with repeated and painful stimulation; verbal output is unintelligible or nil; some purposeful movement to noxious stimulation Comatose : no arousal despite vigorous stimulation, no purposeful movement- only posturing, brainstem reflexes often absent Dementia Confusional state Longstanding nature Acute Varies little from time to time Fluctuate Memory problem Clouding of consciousness Medical or surgical disease Metabolic disorders Hepatic Uremic Hypo and hypernatremia Hypercalcemia Hypo and hyperglycemia Hypoxia Hypercapnia Infectious illness Pneumonia Endocarditis Urinary tract infection Peritonitis Congestive heart failure Postoperative and posttraumatic states Drug intoxication Opiates Barbiturates Other sedatives Diseases of nervous system Cerebrovascular disease, tumor, abscess Subdural hematoma Meningitis Encephalitis Cerebral vasculitis Hypertensive encephalopathy causes of confusional state (5) •Alcoholism. •Depression. •Diabetes. •Drug overdose •Head injuries •Encephalitis •Epilepsy •Stroke History --- emphasizing the patient’s condition before the onset of confusion Clinical examination --- focus on signs of diminished attentiveness, disorientation, and drowsiness and the presence of localizing neurological signs - Control underlying medical illness Quiet the patient and protect him from injury Discontinue drugs that could possibly be responsible for the acute confusional state : sedating, antianxiety, narcotic, anticholinergic, antispasticity, corticosteroid, L-dopa, metoclopramide, cimetidine, antidepressant, antiarrhythmic, anticonvulsant, antibiotics. - - Haloperidol, quetiapine, risperidone are helpful in calming the agitated and hallucinating patient, but should be used in the lowest effective doses In alcohol or sedative withdrawal— chlordiazepoxide is the drug of choice. Chloral hydrate, lorazepam, and diazepam are equally effective Eye opening: Nil To pain (applied to limbs) To voice (including command) Spontaneous (with blinking) 1 2 3 4 Motor response: Nil Arm extension to pain (nail bed pressure) Arm flexion to pain (nail bed pressure) Arm withdrawal from pain (nail bed pressure) Hand localizes pain(supraorbital or chest pressure) Obeys commands 1 2 3 4 5 6 Verbal response: NIL Groans (no re-cognizable words) Inappropriate words (including expletives) Confused speech Orientated 1 2 3 4 5 Glasgow Coma Scale : Eye opening (E) Glasgow Coma Scale : Motor response (M) Glasgow Coma Scale : Verbal response (V) GLASGOW COMA SCORE Notes 1. 2. 3. 4. 5. scoring from the best response verbal response will not correct in the condition of aphasia, intubation and facial injury sensory loss may interfere painful stimulation eye opening may be interfered by orbital swelling and 3rd CN palsy arm movements may be impaired from local trauma or cervical cord lesion History Circumstances and rapidity with which neurologic symptoms developed Immediately preceding medical and neurologic symptoms Use of medications, illicit drugs, or alcohol Chronic liver, kidney, lung, heart, or other medical disease Vital sign Temperature Fever Hypothermia -- <31°C causes coma Pulse Respiratory rate and pattern Blood pressure Funduscopic examination Cutaneous lesion Observe Movement : restless, twitching, multifocal myoclonus, asterisks Decorticate rigidity Suggest severe bilateral damage rostral to midbrain Decerebrate rigidity Indicate damage to motor tracts in the midbrain or caudal diencephalon Level of arousal and elicited movements Brainstem reflexes pupils Ocular movements respiration DESCRIPTIONS Small, reactive INTERPRETATION Metabolic causes Diencephalic lesion Midposition, fixed Mid brain lesion large, fixed Pin point Unilateral fixed dilated Extensive brain stem lesion Anoxia Sedative overdose Anticholinergic poisoning or mydriatic eyedrops Pontine lesion Opiates Third nerve palsy Doll’s eye maneuver (Oculocephalic reflex) Cold caloric test (Oculovestibular reflex) Condition Awake Cerebral dysfunction, brainstem intact Brain stem lesion Doll’s eyes Negative Positive Condition Awake Cerebral dysfunction, brainstem intact Brain stem lesion Cold calorics Nystagmus, N/V, pain Negative Slow deviation toward water Negative Respiratory patterns Cheyne-Stokes respiration : bilateral cortical or bilateral thalamic lesions, metabolic disturbances, incipient transtentorial herniation Hyperventilation : midbrain or pons lesions Apneusis : lateral tegmentum of lower half of pons Cluster : lower pontine or high medullary lesions Ataxic : dorsomedial medulla lesion Least useful sign because : Acid-base derangements Hypoxia Cardiac influences Brain death Locked-in syndrome Vegetative state Frontal lobe disease Non-convulsive status epilepticus Psychiatric disorder (catatonia, depression) An awake but unresponsive state Extensive damage in both cerebral hemisphere Retained respiratory and autonomic functions Cardiac arrest and head injury are the most common causes. Awake patient has no means of producing speech or volitional limb, face and pharyngeal movements Vertical eye movement and lid elevation remain unimpaired Infarction or hemorrhage of the ventral pons COMA LOCALIZING SIGN NO LOCALIZING SIGN SUPRATENTORIAL INFRATENTORIAL - CVD - TUMOUR - ABSCESS STIFF NECK NO STIFF NECK STRUCTURAL DAMAGE - HYPOXIA - CARDIAC ARREST - ENCEPHALITIS - SAH - MENINGITIS FUNCTIONAL NEURONAL DEPRESSION - HEPATIC - URAEMIC - POST ICTAL STATE - FLUID ELECTROLYTE IMBALANCE - DRUGS CBC FBS BUN, Creatinine Electrolyte, calcium LFT Drug screen, toxicology screen EKG CT or MRI brain CSF exam EEG Recovery from coma depends primarily on the causes, rather than on the depth of coma Intoxication and metabolic causes carry the best prognosis Coma from traumatic head injury far better than those with coma from other structural causes Coma from global hypoxic-ischemic carries least favorable prognosis At 3rd day, no papillary light reflex or GCS < 5 is associated with poor prognosis Central transtentorial herniation Brain Herniation Uncal transtentorial herniation Intubation and hyperventilation (PCO2 25-30 mmHg) Mannitol (0.5-1 gm/kg body weight or 20% mannitol 200 cc. infusion 10-20 minutes repeat every 4 hours if necessary Furosemide 20-40 mg IV Dexamethasone 4-10 mg IV q 6 hours decrease perilesional vasogenic cerebral edema. Active at 24-48 hours. Consult surgery