Objectives 44 - U
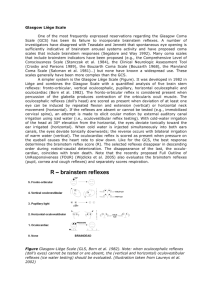
advertisement
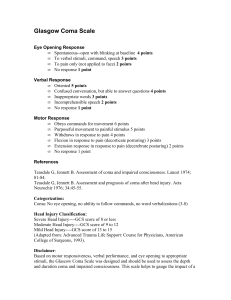
1. Glasgow Coma Scale – describes level of consciousness in a patient - depends on physical examination of three domains: motor ability/response, verbal output/response, and eye opening - scores range from 3-15; Coma defines with score of 8 or less 2. Progression of Coma - expanding intracranial lesion produces a pattern of worsening neurological function of deepening coma - signs of deepening coma can be used to assess the need for acute medical or surgical intervention - depth of coma can be monitored by close monitoring of the respiratory pattern, eye findings, and motor examination - progression of a coma reflects dysfunction of brain structures in a rostral to caudal fashion, ultimately ending with dysfunction of medulla Respiratory patterns - hemispheric dysfunction Cheyne-Stokes breathing, which is a cyclical breathing pattern in which the depth of respiration varies in a smooth wave-like fashion with a periodicity of 1 or 2 minutes - as coma deepens there may be a central hyperventilation pattern in which the depth and frequency of respiration is abnormally high without variation; common cause is pulmonary pathology or metabolic acidosis - further deterioration apneustic breathing pattern in which there is a deep breath which is held for a prolonged period - further deterioration chaotic breathing pattern, ultimately leading to failure of the respiratory drive (agonal) Eye findings - presence of partial or complete unilateral CNII palsy tentorial herniation - mid-position fixed pupils midbrain involvement - large, fixed pupils tectal involvement - pin-point pupils pontine process - pupillary light reflex depends on an arc that passes through the superior colliculi and then into the Edinger-Westphal nucleus; lesions in tectum or midbrain abolish pupillary constrictor response to light large, fixed pupils - lesion in the pons (w/ sparing of midbrain structures) interfere with descending sympathetic pathways originating in hypothalamus alters balance between sympathetic and parasympathetic system leading to pupillary constrictions (Horner’s) - overdose of opioid pin-point pupils (distinguish by administering opioid antagonist) Motor findings - as descending CST influences are lost postural reflexes generated in brainstem become disinhibited - emergence of reflexes is called posturing (abnormal tone in limbs) - posturing reflexes provoked by noxious stimulation, but can also occur spontaneously - misinterpreted as seizure - rostral brainstem intact decorticate posturing flexion of arms and extension of legs; reticulospinal (upper extremity flexing) and rubrospinal tracts - extension of lower extremities driven by driven by disinhibited output of vestibular nuclei while flexion of the upper extremities is driven by the reticulospinal tract - as coma deepens extension of upper and lower extremities with internal rotation of arms; due to loss of descending influences from upper medulla and reflect disinhibited output of the vestibular nuclei (vestibulospinal tract, decerebrate) - finally, as coma progresses to the point where the vestibulospinal outflow if impaired limbs become flaccid 3. Sleep - patients can be aroused from sleep - active brain state with a complicated architecture and different stages, each of which has its own EEG pattern - little or no diminution in cerebral blood flow Coma - a sleep-like state from which a person cannot be aroused - decreasing level of consciousness - EEG pattern in coma does not have stages (as in sleep) and is characterized by abnormally slow frequencies and abnormally low voltages - abnormal decrease in blood flow to the brain Brain Death - no brain activity including most basic brainstem reflex functions To be declared brain dead: - no brainstem reflexes present, including pupillary light reflex, corneal reflexes, and vestibuloocular reflex - apnea in face of a high CO2 level; if medulla is intact, high concentration of carbon dioxide will trigger an automatic breathing response - electrical silence on EEG - absence of blood flow - absence of condition which can stimulate brain death, such as presence of CNS depressant drugs, reversible metabolic lesions, or hypothermia Persistent Vegetative State - irreversible damage that does not lead to death - return of sleep/wake cycles - eyes may open and fixate - brainstem behaviors like yawning, crying, grimacing, and grasping return - level of consciousness improves, but content of consciousness does not improve - absence of learning, meaningful communication, and purposeful movement - cortical function has been permanently disrupted 4. Transtentorial herniation - rostral portion of ascending reticular activating system located in midbrain and diencephalon are critical for maintaining consciousness - lesion in one of the cerebral hemispheres depresses level of consciousness by putting pressure on the brainstem - herniation of brain substance (uncus of temporal lobe) under the tentorium cerebelli - transtentorial herniation occurs when the uncus of the temporal lobe is forced under the tentorium pressure on ipsilateral third nerve CN III palsy - further pressure on the brainstem then impinges on the ascending reticular activating system leading a depressed level of consciousness - as brainstem is shifted toward contralateral side cerebral peduncles forced against opposite edge of the tentorium leading to a hemiparesis that is ipsilateral to the side of the lesion Other cause of coma - bilateral hemispheric process - sub-falcine herniation occurs when an expanding cerebral hemisphere is forced under the falx cerebri, putting pressure on the opposite hemisphere leads to bihemispheric dysfunction and coma