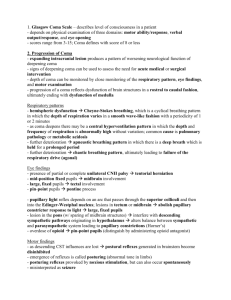
ppt. file
advertisement

Management of comatose patient DR.H.N.SARKER MBBS,FCPS,MRCP(UK), FRCP(Edin) Associate Professor Medicine Introduction Consciousness means wakefulness with awareness of self and surroundings. The state of consciousness is the product of complex interactions between parts of the reticular activating system in brainstem and medial part of thalamus , cortex, and all sensory stimuli. Introduction For a person, in order to maintain consciousness, the two important neurological components must function perfectly. The first is the cerebral cortex which is the gray matter covering the outer layer of the brain, and the other is a structure located in the brainstem, called reticular activating system (RAS or ARAS). Introduction Injury to either, or both of these components is sufficient to cause a patient to experience altered consciousness. Introduction Introduction Altered / Disturbed consciousness: definitions of some terms■ Clouding of consciousness – means reduced wakefulness and/or selfawareness, sometimes with confusion. ■ Confusion means that the subject is bewildered and misinterprets his/her surroundings. ■ Delirium is a state of confusion, sometimes with visual hallucination, and often high arousal (e.g. delirium tremens, ). Introduction ■ Sleep is normal mental and physical inactivity: the subject can be roused. ■ Stupor is abnormal; a sleepy state from which the subject can be aroused by vigorous or repeated stimuli. The term is also used for psychiatric states, e.g. catatonic and depressive stupor. ■ Coma means unrousable unresponsiveness. Coma is a state of unconsciousness whereby a patient cannot react with the surrounding environment. Mechanisms of coma Altered consciousness is produced by three mechanisms affecting brainstem, reticular formation and cortex. ■ Diffuse brain dysfunction. Generalized severe metabolic or toxic disorders (e.g. alcohol, sedatives, uraemia, septicaemia) depress overall brain function. Mechanisms of coma ■ Direct effect within the brainstem. A brainstem lesion inhibits the reticular formation. ■ Pressure effect on the brainstem. A mass lesion within the brain compresses the brainstem, inhibiting the reticular formation. Mechanisms of coma A single focal hemisphere (or cerebellar) lesion does not produce coma unless it compresses or damages the brainstem. Causes of coma Principal causes of coma Diffuse brain dysfunction Drug overdose, alcohol abuse CO poisoning, anaesthetic gases Hypoglycaemia, hyperglycaemia Hypoxic/ischaemic brain injury Hypertensive encephalopathy Causes of coma Diffuse brain dysfunction Severe uraemia Hepatocellular failure Respiratory failure with CO2 retention Hypercalcaemia, hypocalcaemia Hypoadrenalism, hypopituitarism and hypothyroidism Causes of coma Diffuse brain dysfunction Hyponatraemia, hypernatraemia Metabolic acidosis Hypothermia, hyperpyrexia Trauma to brain Epilepsy Causes of coma Diffuse brain dysfunction Encephalitis, cerebral malaria, septicaemia Subarachnoid haemorrhage Metabolic rarities, e.g. porphyria Cerebral oedema from chronic hypoxia Causes of coma Direct effect within brainstem • Brainstem haemorrhage or infarction • Brainstem neoplasm, e.g. glioma • Brainstem demyelination • Wernicke–Korsakoff syndrome • Trauma Causes of coma Pressure effect on brainstem • Hemisphere tumour, infarction, haematoma, abscess, • encephalitis or trauma • Cerebellar mass Causes of coma Common causes of coma (remember by MnomonicAEIOU,DAMM ) • A-Alcohol, Abscess • E- Epilepsy, Encephalitis, Endocrine and Electrolyte disturbance • I- Head injury, Brainstem Infarction or haemorrhage Causes of coma O-Opium,drug Overdose U- Uraemia D- Diabetes(Hypoglycaemia, diabetic ketoacidosis, nonketotic hyperosmolar hyperglycemia) Causes of coma A-Apoplexy, Epidural and subdural hemorrhage, Subarachnoid hemorrhage M- Meningitis,cerebral Malaria M-Metabolic(hepatic failure) Causes of coma A-Apoplexy, Epidural and subdural hemorrhage, Subarachnoid hemorrhage M- Meningitis, cerebral Malaria M-Metabolic (hepatic failure) Approach to the Patient: Coma Immediate assessment Actions that take seconds save lives. • Assess airway, breathing, circulationresuscitate. • Give 100% O2, monitor pulse oximetry and obtain venous access. • Withdraw blood for glucose, other biochemical parameters and drug screening Immediate assessment Record the GCS and check the pupil size and reaction. Check the bedside glucose and the temperature. Consider the differential diagnosis. Look for a Medic alert bracelet or necklace. Immediate therapy If hypoglycaemia, give 50 ml 50% glucose i.v. If hypothermia, start rewarming. If pupils are small, R rate is low or signs of drug abuse are present, give 400µg of naloxane i.v stat and repeat. Subsequent management After initial therapy, subsequent assessment is done by taking history and physical examination including General and neurological examination History All possible information from Relatives Paramedics Ambulance crew Bystanders History Particularly about the mood of onset and circumstances Previous medical historyepilepsy, DM, drug history Clues obtained from pt’s clothing and handbag Examination A thorough examination of all systems is essential but concentrate on the following. 1.Trauma requires complete exposure and roll to examine back 2. Neddle mark Examination 3. Severity of coma-assessed by Glasgow Coma Scale Eye opening (E) • Spontaneous • To speech • To pain • No response 4 3 2 1 Examination Motor response (M) • Obeys • Localizes • Withdraws • Flexion • Extension • No response 6 5 4 3 2 1 Examination Verbal response (V) • Orientated • Confused conversation • Inappropriate words • Incomprehensible sounds • No response 5 4 3 2 1 Examination Glasgow Coma Scale = E + M + V (GCS minimum = 3: maximum = 15) Examination Examination Examination 4. Pupil size and reaction- Examination 5.Spontaneous eye movementAbnormal conjugate deviation suggests intracerebral damage. Dysconjugate deviation implies damage to 3,4 or 6th nerve palsy Examination 6.Respiratory rate and pattern- Examination 7. Signs of Lateralisation suggest focal neurological damage Examination Investigations Often, the cause is evident (e.g. head injury, cerebral haemorrhage, self-poisoning); if no cause is evident, further investigations are essential. Investigations Blood and urine ■ Drugs screen (e.g. salicylates, diazepam, narcotics, amfetamines). ■ Routine biochemistry (urea, electrolytes, glucose, calcium, liver biochemistry). ■ Metabolic and endocrine studies (TSH, cortisol). ■ Blood and urine cultures. ■ Other, e.g. cerebral malaria (request thick blood film). Investigations Imaging CT or MR brain imaging may indicate an unsuspected mass lesion or intracranial haemorrhage. CSF examination Lumbar puncture should be performed in coma only after careful risk assessment. It is contraindicated when an intracranial mass lesion is a possibility: Investigations CT is essential to exclude this. CSF examination is likely to alter therapy only if undiagnosed meningoencephalitis or other infection is present. Electroencephalography EEG is of some value in the diagnosis of metabolic coma and encephalitis. Management Comatose and stuporose patients – at home or outside, on a trolley, in a ward or ITU – need immediate careful nursing, • meticulous attention to the airway (protected airway) , and • frequent monitoring of vital functions and high flow O2. Management Longer-term essentials are: ■ skin care – turning (to avoid pressure sores and pressure palsies), removal of jewellery, a suitable pressure-relieving mattress. ■ oral hygiene – mouthwashes, suction ■ eye care – prevention of corneal damage (lid taping, irrigation) Management ■ fluids – intragastric or i.v. ■ calories – liquid diet through a fine intragastric tube, 3000 kcal daily ■ sphincters – catheterization when essential ; rectal evacuation. Management Broad spectrum antibiotics and/or antivirals should be given empirically if there is any suggestion of bacterial infection or encephalitis . Half-hourly neuro-observations. Management Specific treatmentTreatment of specific causes of coma.