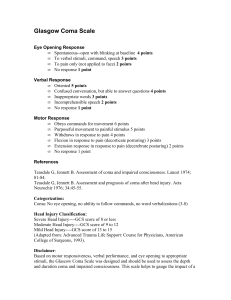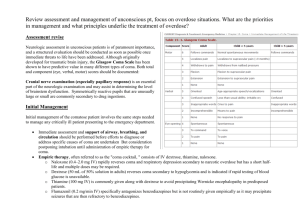
SCHOOL:SCHOOL OF MEDICINE AND CLINICAL SCIENCES PROGRAME: CLINICAL MEDICINE GENERAL NAME : STEVEN BANDA ID NUMBER :21O1O2009 LECTURER: DR C PHIRI COURSE :MEDICINE QUESTION: Discuss How you will take the relevant history for the patient brought to your consultation room in coma INTRODUCTION Medical history taking is a skill necessary form of examination which includes an injury into patients’ medical history, social history, allergies, and medications the patient is taking or may have recently stopped taking. History taking plays an important role for making an accurate diagnosis. In a complete patient history, the following must be considered; • Presenting complaints • History of presenting complaints • Past medical history • Drug history • Family history • Social history It is important to introduce yourself, identify your patient and gain a consent to speak with them. However, taking history in a patient who is in a coma is a bit different from the patient who is conscious. In this case a Glasgow coma scale is used to determine the levels of consciousness. COMA is defined as the state of prolonged unconsciousness with loss of reaction to external stimuli.in this case I am going to discuss on how to take history in a patient who in coma. Causes of coma Metabolic Neurological • Drugs intoxication Trauma • Poisoning (alcohol) Meningitis • Hypoglycemia and hyperglycemia Tumor • Hypoxia, (co2 increase) vascular/ stroke • Septicemia Epilepsy If a patient has been present to your institution in the state of coma, the first thing you should do is to check for the ABC. A. Airway B. Breaths C. Circulation Protect the airway the airway is the most important in this patient consider intubation when the Glasgow coma scale is less than 8. Intubation is the process of inserting a tube into the mouth or nose and then into the airway to help move air in and out of the lung. GCS also to assess the severity of coma in a patient and it will determine which types of acute medical conditions and trauma is it .This scale will give a patient a score according to their verbal and physical responses and how easily they can open their eyes. Therefore, Medical history supposed to be done.. Medical history Would ask friends, family, police, and witnesses some relevant questions: • The onset and time course of the problem (e.g., whether seizure, headache, vomiting, head trauma, or drug ingestion was observed) • Baseline mental status • Recent infections and possible exposure to infections • Recent travel • Ingestions of unusual meals • Psychiatric problems and symptoms • Prescription drug history • Use of alcohol and other recreational drugs (e.g., anaesthetics, stimulants, depressants) • Previous and concurrent systemic illnesses, including new-onset heart failure, arrhythmias, respiratory disorders, infections, and metabolic, liver, or kidney disorders • The last time the patient was normal • Any hunches they may have about what might be the cause (e.g., possible occult overdose, possible occult head trauma due to recent intoxication) Medical records should be reviewed if available. BRIEF COLLATERAL HISTORY 1.How was the patient found 2.When was the patient last seen to be okay 3. Was it abrupt or gradual onset 4 Is there any suggestion of trauma 5.Is there any history of flits when the patient become unconscious 6. Was there any recent complaints like headaches, fever, and depression 7. foreign travel or infection 8. Drugs or toxin exposure that the patient has taken PHYSICAL EXAMINATION Physical examination should be focused and efficient and should include thorough examination of the head and face, skin, and extremities. Signs of head trauma, If unstable injury and cervical spine damage have been excluded, passive neck flexion is done and stiffness suggests subarachnoid haemorrhage or meningitis. INVESTIGATIONS 1. Labs 2. Imaging For labs do the Blood sugar, FBC, Urine Analysis etc. For imaging do the CXR, CT SCAN, LUMBAR PUNCTURE, ECG etc. DIAGNOSIS • History • General physical examination • Neurologic examination, including eye examination • Laboratory tests (e.g., pulse oximetry, bedside glucose measurement, blood and urine tests) • Immediate neuroimaging • Sometimes measurement of ICP • If diagnosis is unclear, lumbar puncture or electroencephalography MANAGEMENT 1. Give oxygen therapy 2. Give glucose if the patient is hypoglycemia 3. Give narexone 4. 5. Give iv thiamine Septic specifics, give cefotoxine 2g bd 6. Suspect malaria give artemethes, quinine 7. Encephalitis; give acyclovir CONCLUSION All in all, Coma is produced by disorders that affects both cerebral hemispheres or the brainstem reticular activiting system. The possible cause of coma is limited: Mass lesion, metabolic encephalopathy, infection of the brain and its covering (meningitis) and sub arachnoid hemorrhage and coma is a life-threatening condition. REFFERENCE 1. www.mayoclinic.org 2. www.webmd.com 3. www.healthline.com 4. www.emedicinehealth.vic.gov.a