Management of unconscious patient
advertisement

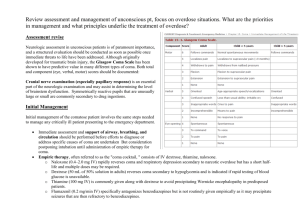
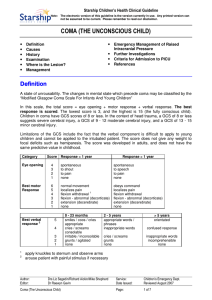
Management of unconscious patient Özlem Korkmaz Dilmen Associate Professor of Anesthesiology and Intensive Care Cerrahpasa School of Medicine Learning Objectives • Definition of unconsciousness • Common causes • Diagnosis and treatment of unconscious patient Definition Unconsciousness is a state in which a patient is totally unaware of both self and external surroundings, and unable to respond meaningfully to external stimuli. A system of upper brainstem and thalamic neurons, the reticular activating system and its broad connections to the cerebral hemispheres maintain wakefulness. Common Causes I • Interruption of energy substrate delivery a. Hypoxia b. Ischemia c. Hypoglycemia • Alteration of neurophysiologic responses of neuronal membranes a. Drug intoxication b. Alcohol intoxication c. Epilepsy Common Causes II • Abnormalities of osmolarity a. Diabetic ketoacidosis b. Nonketotic hyperosmolar state c. Hyponatremia • Hepatic encephalopathy • Hypertensive encephalopathy • Uremic encephalopathy Common Causes III • • • • Hypercapnia Hypothyroidism Hypothermia Hyperthermia An unconscious case • 46 years old, male • DM • Unconscious First Aid • A (Airway) • B (Breathing) • C (Circulation) • D (Disability) • E (Exposure) Airway - A • Head tilt, chin lift • Jaw trust Airway - A • Clearance (aspiration) • Oral/Nasal Airway • Intubation Breathing - B • Look, listen and feel for NORMAL breathing. Breathing - B • Symmetry • Breathing Sounds • Tidal Volume • Respiratory rate Abnormal breathing • Occurs shortly after the heart stops in up to 40% of cardiac arrests • Described as barely, heavy, noisy or gasping breathing • Recognise as a sign of cardiac arrest Circulation - C • Pulse • Rate • Rhytme • Arterial Pressure • Hypertension • Hypotension Disability - D • Disability is determined from the patient level of consciousness according to the AVPU or GCS. A for ALERT V for VOICE P for PAIN U for UNRESPONSIVE to any stimulus GLASGOW COMA SCALE •I. Motor Response •II. Verbal Response 6 - Obeys commands fully 5 - Alert and Oriented 5 - Localizes to noxious stimuli 4 - Confused, yet coherent, speech 4 - Withdraws from noxious stimuli 3 - Inappropriate words and jumbled 3 - Abnormal flexion, i.e. decorticate phrases consisting of words posturing 2 - Incomprehensible sounds 2 - Extensor response, i.e. 1 - No sounds decerebrate posturing •III. Eye Opening 1 - No response 4 - Spontaneous eye opening 3 - Eyes open to speech 2 - Eyes open to pain 1 - No eye opening Exposure an Environment - E The patient’s clothes should be removed or cut in an appropriate manner so that any injuries can be seen. General Physical Examination • History • Neurologic examination • The eye examination • Fundoscopy • Ventilatory pattern History • In many cases, the cause of coma is immediately evident; - Trauma - Cardiac arrest - Drug ingestion • . In the reminder, historical information may be helpful. Cirrhosis Meningococcemic rashs Evolution of neurologic signs in coma from a hemispheric mass lesion as the brain becomes functionally impaired in a rostral caudal manner. Early and late diencephalic levels are levels of dysfunction just above (early) and just below (late) the thalamus. Neck rigidity Neck rigidity • Bacterial meningitis • Subarachnoid hemorrhage Hepatic coma The eye examination Pupillary abnormality is one of the cardinal features differentiating surgical disorders from medical disorders. Pupillary abnormalities in coma generally herald structural changes in brain, whereas in metabolic coma such abnormalities are not present. Fixed and dilated pupils Fixed and dilated pupils • The terminal stage of brain death • Atropine effect Pinpoint pupils Pinpoint pupils • Narcotic overdose • Bilateral pontine damage Pupillary dilatation Pupillary dilatation Sudden lesion of the midbrain; ruptere of an internal carotid artery aneurysm Fundoscopic examination Fundoscopic examination • Subarachnoid hemorrhages • Hypertensive ensefalopaty • Increased inrtacranial pressure Laboratory examination Chemical blood determinations are made routinely to investigate metabolic, toxic or drug induced encephalopaties. -Electrolytes -Calcium -Blood urea nitrogen -Glucose -NH3 Laboratory examination • Toxicological analysis is of great value in any case of coma where the diagnosis is not immediately clear. • The presence of alcohol does not ensure that alcohol is the cause of the altered mental status. Other, life-threatening, causes must be ruled out. Imaging • In coma of unknown etiology, CT or MRI must be performed. • Radiologically detectable causes of coma; - Hemorrhage - Tumor - Hydrocephalus Brain herniation Electroencephalography EEG is useful in unrecognized seizures. Lumbar puncture • The use of LP in coma is limited to diagnoses of meningitis and instances of suspected subarachnoid hemorrhage in which the CT is normal. Complaints History of diabetes, use of oral Diagnosis * Hypoglycaemia Action • *Test blood for glucose using anti-diabetic or ingestion of test strip or glucose meter. alcohol • Give IV Glucose History of ingestion of Drug overdose. • Support respiration medication (tablets or liquid). e.g. Alcohol, • IV Glucose to prevent There may be smell of alcohol hypoglycaemia. or other substance on breath In chronic alcoholics • Precede IV glucose with IV Thiamine, IV fluid administration. E.g. Paracetamol. • Gastric lavage, nacetylcysteine treatment if > 140 mg/kg body weight ingested Complaints Diagnosis Action Presence or absence of history * Diabetic ketoacidosis • *Give Soluble Insulin and of diabetes; Sodium Chloride 0.9% infusion - polyuria, polydipsia - hyperventilation - gradual onset of illness - evidence of infection - Urine sugar and ketone positive - Blood glucose> 250 mg/dL Fever, fits, headache, neck * Meningitis or Cerebral Malaria • *Treat with antibiotics and stiffness, altered quinine until either diagnosis consciousness etc confirmed. History of previous fits, sudden * Epilepsy • *Give Diazepam, IV, to abort onset of convulsions; with or fits and continue or start with without incontinence. anti-epileptic drug treatment Complaints Patient with hypertension or diabetes; sudden onset of Diagnosis * Stroke Action • Check blood pressure and blood glucose. paralysis of one side of body. Patient with hypertension, headaches, seizures * Hypertensive encephalopathy • Check blood pressure • If very high, give oral or parenteral anti-hypertensives Thank you for your attention