male & female HISTOLOGY LECTURE & lab
advertisement
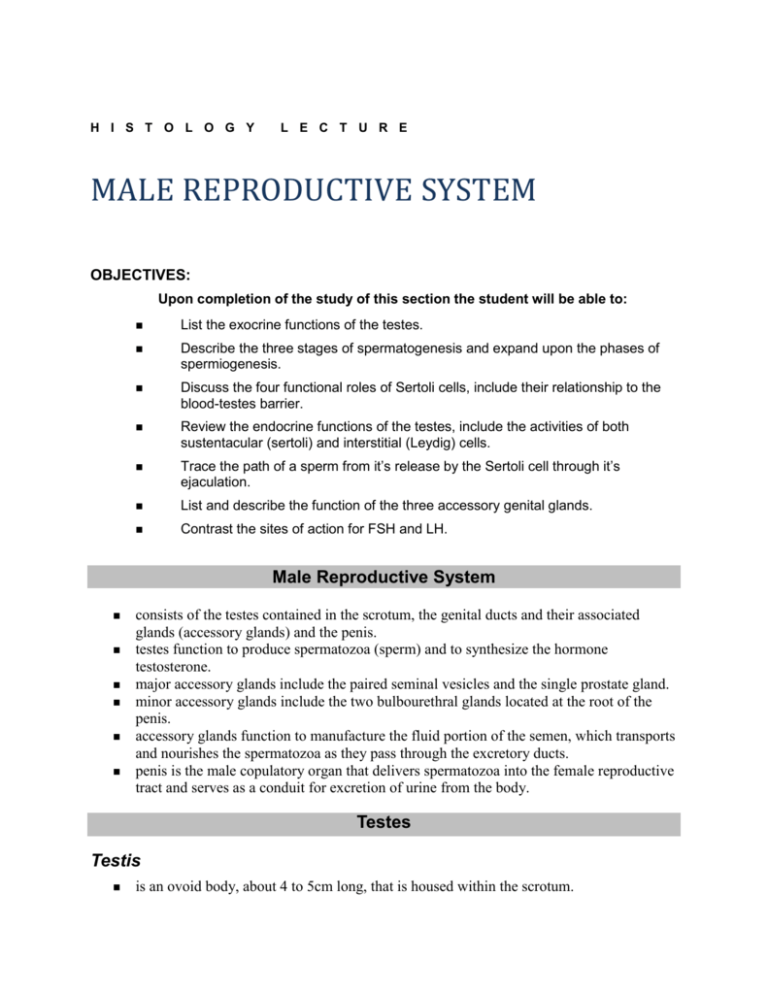
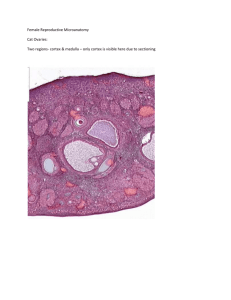
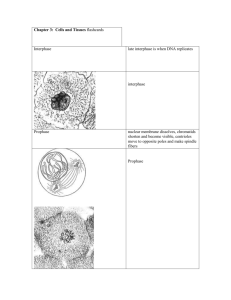
H I S T O L O G Y L E C T U R E MALE REPRODUCTIVE SYSTEM OBJECTIVES: Upon completion of the study of this section the student will be able to: List the exocrine functions of the testes. Describe the three stages of spermatogenesis and expand upon the phases of spermiogenesis. Discuss the four functional roles of Sertoli cells, include their relationship to the blood-testes barrier. Review the endocrine functions of the testes, include the activities of both sustentacular (sertoli) and interstitial (Leydig) cells. Trace the path of a sperm from it’s release by the Sertoli cell through it’s ejaculation. List and describe the function of the three accessory genital glands. Contrast the sites of action for FSH and LH. Male Reproductive System consists of the testes contained in the scrotum, the genital ducts and their associated glands (accessory glands) and the penis. testes function to produce spermatozoa (sperm) and to synthesize the hormone testosterone. major accessory glands include the paired seminal vesicles and the single prostate gland. minor accessory glands include the two bulbourethral glands located at the root of the penis. accessory glands function to manufacture the fluid portion of the semen, which transports and nourishes the spermatozoa as they pass through the excretory ducts. penis is the male copulatory organ that delivers spermatozoa into the female reproductive tract and serves as a conduit for excretion of urine from the body. Testes Testis is an ovoid body, about 4 to 5cm long, that is housed within the scrotum. develops retroperitoneally in the abdominally cavity and descends into the scrotum, carrying parietal and visceral layers of the peritoneum (the tunica vaginalis) that partially cover the testis on its anterior and lateral surfaces. Tunica Albuginea is the thick fibrous connective tissue capsule of the testis. is thickened posteriorly to form the mediastinum testis from which connective tissue septa arise to divide the organ into approximately 250 compartments (lobuli testis). Lobule Testis are pyramidal-shaped incomplete compartments that intercommunicate. contain from 1 to 4 seminiferous tubules each, embedded in a meshwork of loose connective tissue where nerves, vessels, and scattered interstitial cells of Leydig are present. Interstitial Cells of Leydig are located in the interstitial spaces between the seminiferous tubules. mature and begin to secrete during puberty and are richly supplied with capillaries and lymphatic vessels. are round to polygonal in shape, possessed a large central nucleus, many mitochondria, a well-developed Golgi apparatus, and many lipid droplets. are endocrine cells that produce the male sex hormone testosterone, when stimulated by luteinizing hormone (interstitial cell stimulating hormone) from the pituitary gland. Seminiferous Tubules are the sites where spermatozoa are produced. are 30 to 70 cm long, with a diameter of 150 to 250 um. are lined by a complex, stratified epithelium. are enveloped by a fibrous connective tissue tunic, composed of several layers of fibroblasts. Myoid cells, resembling smooth muscle, are present in the inner layer of some species, but not in humans. form tortuous pathways through the organ before they become continuous with the short straight tubuli recti. Tubuli Recti have a narrow lumen lined by a simple cuboidal epithelium. lead into the rete testis, a network of epithelial-lined channels located in the mediastinum. Ductuli Efferentes lead from the rete testis into the epididymis. Seminiferous Epithelium is composed of two different types of cells, the spermatogenic cells from which the germ cells eventually develop and the Sertoli cells, which support and provide nutrition to the spermatogenic cells. is 4 to 8 cell layers thick. Sertoli Cells are columnar, extremely complex in shape, and extend from the basal lamina to the lumen. their apical and lateral plasma membranes are markedly irregular in outline since they envelope the developing germ cells. contain a well-developed smooth endoplasmic reticulum, some rough endoplasmic reticulum, an abundance of mitochondria and lysosomes, and an extensive Golgi apparatus. nucleus is pale, oval, displaying frequent indentations and a large nucleolus. form occluding junctions with adjoining Sertoli cells, thus subdividing the lumen of the seminiferous tubule into a basal and an adluminal compartment. zonulae occludentes are responsible for establishing the blood-testis barrier that serves to protect the developing sperm cells from autoimmune reactions. Functions of Sertoli cells are manifold. support, protect, and nourish developing spermatozoa. phagocytose excess cytoplasm discarded by spermatids in the process of spermiogenesis. secrete a fluid into the seminiferous tubules that transports spermatozoa to the genital ducts. contain FSH receptors and under FSH influence synthesize androgen-binding protein (ABP) that binds testosterone, concentrating it to permit sperm maturation. secrete inhibin, a hormone that inhibits synthesis and release of FSH from the anterior pituitary. Spermatogenic Cells include several characteristic cell types in the seminiferous epithelium: spermatogonia, primary spermatocytes, secondary spermatocytes, spermatids, and spermatozoa. each of these cells represents a distinct stage in the differentiation of male germ cells. The entire process is known as spermatogenesis. Spermatogenesis is divided into three phases: spermatocytogenesis, meiosis, and spermiogenesis. in man takes approximately 64 days; its cell divisions are unusual, in that the daughter cells remain connected to each other via intercellular bridges (forming a syncytium). Syncytium may be responsible for the synchronous development of germ cells along any one seminiferous tubule. is disrupted at the completion of spermatogenesis, when the individual spermatozoa are released into the lumen. Spermatocytogenesis refers to division of the spermatogonia to provide a continuous supply of cells that will give rise to primary spermatocytes. Meiosis are two successive divisions that reduce the chromosome number from diploid to haploid and produce spermatids. Spermiogenesis is cytodifferentiation and transformation of spermatids to form spermatozoa. Spermatogonia are the diploid germ cells that sit upon the basal lamina. are of three types: pale type A, dark type A, and type B. Pale Type A are small (about 12 um diameter) and possess a pale-staining nucleus and cytoplasm containing spherical mitochondria, a small Golgi complex, and abundant free ribosomes. at puberty these cells undergo mitosis and give rise to either more pale type A spermatogonia (to maintain the supply of spermatogonia) or type B spermatogonia (which undergo mitosis and give rise to primary spermatocytes). Dark Type A (with dark nuclei) represent noncycling, reserve cells that have the potential to produce more pale type A cells. Primary Spermatocytes are identified as the largest germ cells in the seminiferous epithelium. are diploid cells (46 chromosomes) that undergo meiosis. Prophase of the first meiotic division is long (it takes more than 22 days). including several stages: leptotene, zygotene, pachytene, diplotene (during which crossing over, the exchange of genetic material between homologous chromosomes, occurs) and diakinesis. is followed by metaphase I, anaphase I, and telophase I, which compose the first meiotic division. First Meiotic Division results in the formation of small secondary spermatocytes. Secondary Spermatocytes possess the haploid number of chromosomes (23), and the amount of DNA has been reduced (from 4N to 2N). quickly undergo the second division, producing spermatids. Spermatids are haploid cells with 23 chromosomes and one-half the amount of DNA (since no S phase took place). are small (7 to 8 um diameter) and located near the lumen of the seminiferous tubule. their nuclei often display regions of condensed chromatin. contain a pair of centrioles, mitochondria, free ribosomes, smooth endoplasmic reticulum, and a well-developed Golgi apparatus. undergo the cytodifferentiation process known as spermiogenesis. Spermiogenesis is the unique differentiation process whereby spermatids transform into spermatozoa that are release into the lumen of the seminiferous tubule. acrosome and sperm tail are formed during spermiogenesis, the nucleus becomes condensed and elongated, and excess cytoplasm not directly involved in forming the spermatozoa is shed and phagocytosed by Sertoli cells. is divided into four phases: Golgi, cap, acrosome, and maturation phases. Golgi Phase of spermiogenesis is characterized by the formation of proacrosomal granules in the Golgi complex. Proacrosomal Granules coalesce to form a single acrosomal granule enclosed within an acrosomal vesicle, which becomes attached to the anterior end of the nuclear envelope. Centrioles migrate away from the nucleus to form the flagellar axoneme and then retreat toward the nucleus and assist in forming the connecting piece associated with the tail. Cap Phase involves the expansion of the acrosomal vesicle over much of the nucleus, to form the acrosomal cap. Acrosomes contain hydrolytic enzymes (acid phosphatase, neuraminidase, hyaluronidase, protease, and phosphatase). Acrosomal Reaction refers to the release of enzymes that facilitate the dissociation of the cells of the corona radiata and the digestion of the zona pellucida. Acrosome Phase is characterized by the nucleus becoming condensed and flattened, mitochondria aggregating around the proximal portion of the flagellum to form the middle piece, and elongation of the spermatid. Elongation may be facilitated by a cylinder of microtubules, the manchette. By the end of the acrosome phase the spermatids are oriented with their acrosomes pointing toward the base of the seminiferous tubule. Maturation Phase is characterized by excess cytoplasm being discarded (including the intercellular bridges that connected the spermatids) and phagocytosed by Sertoli cells. is completed when nonmotile spermatozoa are released (tail first) into the lumen of the seminiferous tubule. Cycle of Seminiferous Epithelium refers to the wave-like sequence of maturation that occurs along the seminiferous tubules. One Cycle is the reappearance of identical cell associations within the epithelium. in humans is approximately 16 days, so that four cycles (64 days) must occur for a spermatogonium to be transformed into a spermatozoon. Histophysiology Temperature of 35oC is critical for the development of spermatozoa. is achieved in the scrotum by the pampiniform plexus of veins that wrap around the testicular artery and function to dissipate heat. is achieved also by evaporation of sweat from the skin of the scrotum. below 35oC, contraction of the cremaster muscle in the spermatic cord brings the testis close to the body wall to increase the temperature. Cryptorchidism is a condition when the testes fail to descend into the scrotum during development. the normal body temperature inhibits spermatogenesis, resulting in sterility. However, this condition does not affect testosterone production. Luteinizing Hormone (LH) of the pituitary gland stimulates the interstitial cells of Leydig to secrete testosterone, which is responsible for the normal development of male germ cells and secondary sex characteristics. Follicle-Stimulation Hormone (FSH) of the pituitary gland acts on the Sertoli cells, promoting the synthesis of androgenbinding protein (ABP). ABP binds with testosterone and maintains a high concentration of testosterone in the seminiferous tubules, where it is essential for spermatogenesis. binds estrogens and inhibits spermatogenesis. Increased testosterone levels inhibit LH release, whereas FSH release is stopped by inhibin (secreted by Sertoli cells). Genital Ducts convey the spermatozoa and semen to outside of the body. extend from the seminiferous tubules to the urethra. Although they are continuous, they are structurally and histologically different. Their names identify the regional division and unique characteristics they possess. Tubuli Recti are short straight tubules, located in the mediastinum testis, which convey spermatozoa from the seminiferous tubules to the rete testis. their lumen is lined by a simple cuboidal epithelium having cells that possess microvilli and a single flagellum on their luminal surface. Rete Testis is a labyrinthine plexus of anastomosing channels within the mediastinum testis that connect the tubuli recti with the ductuli efferentes. are lined by a simple cuboidal epithelium, and, like those of the tubuli recti, many of the cells possess a single flagellum. Ductuli Efferentes is a collection of 10 to 20 tubules leading from the rete testis to the ductus epididymis. are lined by a simple epithelium, composed of alternating clusters of (nonaffiliated) cuboidal and (ciliated) columnar cells. Cuboidal Cells possess microvilli, contain lysosomal granules, and function to reabsorb fluid from the semen. Ciliated Columnar Cells aid in transporting the nonmotile spermatozoa toward the epididymis. Smooth Muscle in the form of a thin circular layer underlies the basal lamina surrounding the ductuli efferentes epithelium. Ductus Epididymis begins as the terminal portions of the ductuli efferentes fuse. is a narrow, highly coiled tubule, 4 to 6 meters long. is surrounded by connective tissue containing blood vessels. is subdivided into a head, body, and tail region. its lumen is lined pseudostratified columnar epithelium. Epithelium is composed of basal and principal cells. Basal Cells are round and appear undifferentiated, apparently serving as precursors of the columnar principal cells. Principle Cells possess stereocilia (long irregular branching microvilli) on their luminal surface. also possesses endoplasmic reticulum, a large Golgi complex, lysosomes, and many pinocytotic and coated vesicles in their apical portions (suggesting fluid resorption). secrete glycerophosphocholine, a substance that probably inhibits capacitation. Capacitation is a process whereby the sperm becomes capable of fertilizing the ovum, and, although it begins in the epididymis, it is not completed until the sperm reaches the oviduct. Basal Lamina supports the epithelium and is in turn surrounded by circular layers of smooth muscle, which increase in thickness and undergo peristaltic contractions that move the sperm toward the ductus deferens. Ductus Deferens (vas deferens) begins at the end of the ductus epididymis as a straight tube with a thick muscular wall. Pseudostratified Epithelium (with stereocilia) similar to that of the ductus epididymis, lines the narrow, irregular lumen of the ductus deferens. Muscular Wall is composed of inner and outer layers of longitudinally oriented smooth muscle, separated from one another by a middle circular layer. Ampulla is the dilated portion of the ductus deferens that leads directly to the prostate gland. its epithelium is thickened and greatly folded. its distal end receives the seminal vesicle, thus forming the ejaculatory duct that enters the prostate gland. Ejaculatory Duct is the straight continuous of the ductus deferens beyond where it receives the ducts of the seminal vesicles. lacks a muscular wall. It enters the prostate gland and terminates as a slit on the colliculus seminalis, in the prostatic urethra. Accessory Genital Glands include the seminal vesicles, the prostate gland, and the bulbourethral glands. produce most of the seminal fluid. Seminal Vesicles are the paired tortuous tubular glands (15 cm in length) located adjacent the posterior aspect of the bladder. their ducts join the ductus deferens just prior to its entering the prostate gland. Psuedostratified Columnar Epithelium lines the extensively folded mucosa of this gland. consists of low columnar cells interspersed with cuboidal basal cells (whose height is testosterone dependent). Columnar Cells have many yellow lipochrome pigment granules and secretory granules, contain a large Golgi apparatus, many mitochondria, and an abundant rough endoplasmic reticulum. Lamina Propria consists of fibroelastic connective tissue surrounded by an inner circular and an outer longitudinal layer of smooth muscle. Adventitia is also composed of fibroelastic connective tissue. Secretory Product is a yellow, viscous fluid that is rich in fructose and other substances and constitutes about 70% of the human ejaculate. Prostate Gland surrounds the urethra as it exits the urinary bladder and is the largest accessory gland. consist of 30 to 50 discrete branched tubuloalveolar glands that empty their contents into the prostatic urethra (via excretory ducts). Glands of the Prostate are arranged in three concentric layers (mucosal, and main) around the urethra and are surrounded by a fibroelastic capsule that contains smooth muscle. stroma from the capsule penetrate the gland and divide it into lobes. Simple or Pseudostratified Columnar Epithelium lines the glands, and the fibroelastic connective tissue enveloping them contains elastic fibers and is richly vascularized. Epithelial Cells contain abundant rough endoplasmic reticulum, a well-developed large Golgi complex, numerous lysosomes, and many secretory granules. Prostatic Concretions composed of glycoprotein are sometimes observed in the lumina of the glands. may become calcified and their numbers increase with age. Secretion of the prostate, under the influence of dihydrotestosterone, is a whitish, thin fluid containing proteolytic enzymes, citric acid, acid phosphatase, and lipids. Prostatic Carcinoma induces elevated acid phosphatase blood levels, which is used as diagnostic tool. Bulbourethral Glands (Cowper’s glands) located adjacent to the membranous urethra, empty their clear secretion into the lumen to lubricate it. are lined by a simple cuboidal or columnar epithelium. Wide fibroelastic septa (containing smooth and skeletal muscle cells) extend from the capsule to subdivide the gland into lobules. Penis functions both as an excretory organ for urine and as a copulatory organ for delivering sperm into the female reproductive tract. is composed of three cylindrical masses of erectile tissue. The paired corpora cavernosa lie dorsally and the single corpus spongiosum contains the penile (spongy) urethra. is covered by skin that overlies a loose connective tissue sheath that surrounds the corpora cavernosa and corpus spongiosum. skin (distally) lacks hair follicles and contains only a few sweat glands. hypodermis contains a prominent layer of smooth muscle but no adipose tissue. Prepuce that portion of skin that covers the glans penis. resembles as mucous membrane, since it is lined by stratified squamous nonkeratininzed epithelium. Tunica Albuginea is the thick fibrous connective tissue sheath surrounding the three erectile bodies. The arrangement of the dense collagen bundles in the tunica permit extensibility of the penis during erection. Corpora Cavernosa are the two-paired erectile bodies dorsally in the penis. contain irregular vascular spaces lined by a continuous layer of endothelial cells separated from each other by trabeculae of connective tissue and smooth muscle cells. Vascular Spaces are decreased in size toward the periphery of the corpora. become engorged with blood during erection, making the penis turgid. Corpus Spongiosum is the singular erectile body surrounding the spongy urethra. its erectile tissue is similar to those of the corpora cavernosa, except that the trabeculae contain more elastic fibers and only a few smooth muscle cells. its vascular spaces are uniform throughout. Glands of Littre are mucus secreting glands that are also present throughout the length of the penile urethra. Glans Penis is the terminal end of the corpus spongiosum. contains dense connective tissue and longitudinal muscle fibers. Erection occurs when the erectile tissues become distended with blood due to parasympathetic stimulation mediated by tactile or erotic stimulation. Parasympathetic Impulses constrict arteriovenous shunts and dilate the helicine arteries, which force blood into the spaces of the erectile bodies under pressure, engorging them with blood. Ejaculation and/or termination of erotic stimulation causes diminished parasympathetic activity, followed by detumescence, and the penis returns to the flaccid state. H I S T O L O G Y L A B O R A T O R Y Male Reproductive System OBJECTIVES: Upon completion of study of this section the student will be able to: 1. Identify the endocrine and exocrine subdivisions of the testes. 2. Distinguish the cells of the spermatogenic cell lineage. 3. Identify and distinguish among epididymis, vas deferens, urethra, seminal vesicles and the prostate gland. 4. Describe the structure of the penis and indicate how it becomes tumescent. ANNOTATIONS Refer to the Male Reproductive System handout to review the functions and basic organization of the structures examined in this session. Human testis, H&E (Harris Biol. H.10-66): The structure of the tissues resembles that of a grapefruit, a thick skin beneath which lies membrane separated segments. The testes outer surface is lined by a thin squamous mesothelium beneath, which is a very dense irregular capsule called the tunica albuginea. Connective tissue septa subdivide the interior into about 250 lobular compartments. Centrally the septa merge forming the vascular and nerve rich mediastinum. In each lobular compartment a 2-4 coiled and compacted seminiferous tubules. The tubules are suspended within a loose CT matrix that contains islands of clustered testosterone secreting interstitial (Leydig cells). The seminiferous tubules are surrounded by a layer of flattened myoid cells that are closely applied to the basement membrane. The seminiferous tubule epithelium is stratified (i.e., sperm lineage cells stacked upon Sertoli cell surface). The predominant cell is the large pyramidal Sertoli cell, which possesses a large elliptical nucleus with prominent nucleolus. Large rounded pale cells, with condensed nuclear heterochromatin, toward the luminal side of the myoid cells are type A spermatogonia. The type B-cells possess a larger, more euchromatic nucleus. The next layer of cells toward the lumen are the primary spermatocytes which are the largest cells and their nuclei almost always show condensed chromosomes. Secondary spermatocytes are found closer to the lumen, are about half the size of the primary spermatocytes and are frequently not identifiable because they rapidly divide and form the spermatids, small rounded cells near the lumen with condensed heterochromatin. During spermiogenesis the spermatid nuclei condense and become more pointed. The heads of these forming spermatozoa are embedded in the Sertoli cells and their flagella tails extend into the lumen. Identify and check-off each of the following: ( ) Tunica albuginea ( ) Lobule septum with blood vessels ( ) Interstitial cells ( ) Seminiferous tubules ( ) Sertoli cell ( ) Myoid cell ( ) Type A spermatogonium ( ) Type B-spermatogonium ( ) Spermatozoan ( ) Primary spermatocyte ( ) Secondary spermatocyte ( ) Spermatid Epididymis, H&E: Examine each of the two slides listed compare the structures included in each section, there might be regions of efferent ductules, portions of the vas deferens or rete testes included The epididymus consists of a highly coiled tubule by pseudostratified columnar epithelium. The lining cells possess numerous stereocilia projecting from their apical surfaces. Sperm and detached cells are present in the lumen. The epithelium is contained within a sleeve of smooth muscle. The muscle is thinnest at the proximal end of the epididymus and becomes three thick layers where it becomes continuous with the thick musculature of the vas deferens. Identify and check-off each of the following: ( ) Cross-section of epididymus ( ) Stereocilia ( ) Smooth muscle of muscularis ( ) Spermatozoa Spermatic cord, H&E (Harris Biol. H.10-651): The spermatic cord consists of the vas deferens, blood vessels nerves, the Pampiniform plexus (temperature regulation) and cremaster skeletal muscle fibers. The vas deferens is lined by a pseudostratified columnar epithelium, which sits upon a thick walled muscular tube. There are three muscle layers with cells oriented longitudinally, circularly and longitudinally with respect to the long axis of the duct. Muscular contractions of this duct account for most of the ejaculatory pressure. Look for a plexus of large irregular veins surrounding one or two arteries. This Pampiniform plexus is a counter current exchange-cooling device to lower blood temperature. Look for the striated skeletal muscle of the cremaster muscle. Bundles of basophilic peripheral nerves (in slides from this commercial source, see above) and adipose are found within the loose CT of the cord. Identify and check-off each of the following: ( ) Vas deferens ( ) Pseudostratified columnar epithelium ( ) Muscle tunics ( ) Pampiniform plexus ( ) Skeletal muscle ( ) Artery ( ) Vein Seminal vesicle, H&E (Carolina Biol. H.8700): 5. At low magnification scan the section and identify the complexly folded mucosa lined by a secretory simple epithelium the folds subdivide the lumen into many irregular compartments which are all continuous, centrally. 6. The lining epithelial cells sitting on the lamina propria are anywhere from pseudostratified columnar to low cuboidal in height, depending upon their activity. The cells secrete about 70% of the fructose-rich semen. This organ is characterized by the appearance of the complexly folded lumen and thick muscular coat. Identify and check-off each of the following: ( ) Mucosal folds ( ) CT of lamina propria ( ) Smooth muscle layers Prostate, H&E: The prostate, the largest accessory gland in the male, surrounds the urethra from it origin from the bladder. The gland consists of 30-50 tubuloalveolar glands drained by 20 or more ducts into the prostatic urethra. The gland is enclosed in a CT capsule subdivided by septa. The glands are irregularly organized and the lining epithelium may range from pseudostratified to simple squamous depending on the region and its activity. The lumina of the glands characteristically possess glycoprotein prostatic concretions, which increase with age. The lamina propria surrounding the glands is rich in smooth muscle myocytes. The prostatic urethra is lined by transitional epithelium containing an eosinophilic apical cell layer. The glands are arranged in three strata surrounding the urethra (centrally, beneath the epithelium are periurethral mucosal glands, medially are the submucosal glands and peripherally are the more abundant main prostatic glands. Identify and check-off each of the following: ( ) Prostatic gland ( ) Prostatic concretions ( ) Urethra ( ) Smooth muscle Penis, H&E (Harris Biol. H10-14): 7. Beneath the thin skin and underlying dermis is a rich, more loosely organized hypodermis. 8. The hypodermis contains an abundance of blood vessels and peripheral nerves. Within the dorsal portion of the penile shaft are the two erectile cylinders, the corpora cavernosa of the penis. Each corpus is ensheathed in an unusually dense CT matrix called the tunica albuginea. The erectile tissue consists of large venous sinuses separated by CT trabeculi. 9. The erectile tissue veins are supplied by deep arteries. Beneath the corpora cavernosa of the penis lies the smaller corpus cavernosum of the urethra. Centrally within this erectile tissue is the penile urethra. In my slide there is not much erectile tissue around the urethra, it is mainly comprised of smooth muscle cells. ldentify and check-off each of the following: ( ) Urethra ( ) Deep artery ( ) Erectile tissue ( ) Corpus cavernosum of the penis ( ) Thin skin ( ) Artery ( ) Vein H I S T O L O G Y L E C T U R E FEMALE REPRODUCTIVE SYSTEM OBJECTIVES: The complexity of the female reproductive system is reflected in the diversity of the organs that constitute the system, the interactions of hormones within the system and the relationship of the system with other organs, notably the hypothalamus and pituitary. The health care professional must understand the structure and function of the system in order to treat the clinical problems that are associated with each of the organs of the system. The areas of clinical interest include carcinomas of the breast, ovary, cervix and uterus, benign tumors of the breast and fibroid tumors of the uterine myometrium, management of pregnancies by caring for individuals with normal conception, gestation and delivery and treatment of persons unfortunate to have an ectopic pregnancy or miscarriage, counseling about birth control and hormone replacement therapies. The internal structures of the female reproductive system consist of two ovaries, two oviducts or Fallopian tubes, the uterus, cervix and vagina. External organs include the clitoris, labia majora, labia minora and the glands of the vaginal vestibule. REFERENCES The Female Reproductive System is covered in Chapter 22 in Basic Histology and in Chapter 17 in the Gartner and Hiatt atlas. OVARY The ovaries are paired organs which lie in the peritoneal cavity and are suspended from the mesentery by a connective tissue membrane, the suspensory ligament. The medial poles of the ovaries attach to the uterus by the ovarian ligament. OVARIAN FUNCTIONS The ovaries have two main functions: 1) Production of the female germ cells, the ova (oocytes), by the process of oogenesis. 2) Synthesis and secretion of steroid hormones which regulate the maturation of developing gametes or oocytes and maintain secondary sex organs. STRUCTURE The ovary is divided into an outer cortex made of connective tissue and developing oocytes and inner medulla containing blood vessels and nerves. Oocytes go through progressive developmental stages in the cortex in structures called follicles and usually one ovum per month is released from the ovary at ovulation. After ovulation, the residual supporting cells which remain in the ovaries are transformed into the corpus luteum which persists for a variable length of time. If pregnancy occurs, the corpus luteum continues to function until parturition. If the ovum is not fertilized, the corpus luteum regresses and is infiltrated with fibrous connective tissue to become the corpus albicans. Fibrous connective tissue forms a band of variable width called the tunica albuginea (literally, white coat) which lies under a single layer of cuboidal epithelial cells (arrow) covering the surface of the ovary. This epithelial tissue is given the unfortunate name germinal epithelium. The epithelial coat has nothing to do with the formation of germ cells, but is simply the reflection of the peritoneum over the ovarian surface. FOLLICULAR ORGANIZATION PRIMORDIAL FOLLICLE. Several oocytes in various stages of development are located in the ovarian cortex. The most primitive oocytes are associated with a single layer of flattened peripheral cells in structures termed primordial follicles. Oocyte surrounded by a single layer of squamous cells. The oocyte is called primary oocyte and is in prophase of first meiotic division. The layer of follicular cells arrests further meiotic activity until after the female is sexually mature. Meiosis continues during ovulation and fertilization of the ovum. PRIMARY FOLLICLE : It is the first stage in the development of the growing follicle. Under the influence of follicle stimulating hormone (FSH) from the pituitary, follicles begin their maturation. The peripheral, support cells, also known as follicular or granulosa cells, enlarge to form a single layer of cuboidal cells and the follicle enlarges in size to become the primary follicle. A layer of glycoprotein (zona pellucida) develops around the oocyte. Microvilli from the oocyte and the granulosa cells penetrate the zona pellucida, and this appears, at the light microscopic level, as an increase in stain density in those regions. Communicating junctions between the oocyte and the granulosa cells have been identified by electron microscopy. Connective tissue in the immediate vicinity of the primary follicle is organized into two distinct zones, the theca interna next to the follicular cells and the outer theca externa continuous with the stroma. Cells of the theca interna are steroid secreting cells. They have LH receptors and secrete androgens that are estrogen precursors. As expected the theca interna is a highly vascular structure. Further development of primary follicles results from the mitoses of granulosa cells to produce a multilaminar (many layers of granulosa cells) primary follicle. SECONDARY FOLLICLE The primary follicle continues its maturation and becomes a secondary follicle when a fluid filled cavity displaces the follicular cells (also called granulosa cells). The cavity is known as the antrum, and the follicle is also known as an antral follicle. Several of these cavities form and coalesce into a single large chamber. The oocyte is surrounded by several layers of granulosa cells called the corona radiate and the oocyte rests on a small hill of granulosa cells called the cumulus oophorus. The antrum contains a hormone-rich fluid secreted by the granulosa cells. GRAAFIAN FOLLICLE Continued maturation and enlargement of the secondary follicle form a structure called the Graafian follicle (mature follicle) which exists just prior to ovulation. The follicle is so large that the entire structure is often not entirely included in histologic sections. The oocyte and attendant corona radiata granulosa cells rest on a hill of granulosa cells, the cumulus oophorus. OVULATION : A surge of luteinizing hormone (LH) from the pituitary occurs at midcycle causing increased blood flow to the ovaries, edema and release of collagenase in the vicinity of the mature follicle. The primary oocyte completes the first meiotic division to form the secondary oocyte and first polar body. The secondary oocyte enters the second meiotic division and stops at metaphase. The secondary oocyte and surrounding granulosa cells are released from the ovary. CORPUS LUTEUM : At ovulation with the release of the ovum and loss of antral fluid, rearrangement of the granulosa cells and theca interna cells occurs. Hormones from the corpus luteum (CL) inhibit pituitary LH and FSH preventing ovulation of other follicles. If the individual becomes pregnant, the corpus luteum is maintained for 4-5 months by placental human chorionic gonadotropin (HCG). If pregnancy does not occur, the corpus luteum degenerates. GRANULOSA LUTEIN CELLS : Granulosa cells fill the collapsed antrum and are known as granulosa lutein cells. These are large, round cells with a central nucleus. They convert androgens from theca lutein cells into estrogens which they secrete. They also secrete progesterone. THECA LUTEIN CELLS: The cells of the theca interna retain their linear characteristics, are called theca lutein cells, are interspersed between the granulosa lutein cells and are fewer in number. They secrete progesterone and androgens. CORPUS ALBICANS : Degeneration of the corpus luteum produces a structure which is invaded by fibroblasts and phagocytic cells. The corpus luteum becomes fibrotic and the cells are removed by macrophages resulting in a white scar in the ovary, hence the name corpus albicans. ATRETIC FOLLICLE : Usually one ovum is released from the ovary at ovulation. However, a number of primordial follicles responded to FSH (or to local factors) and develop concurrently with the follicle that undergoes ovulation. These remain in the ovary and degenerate to form atretic follicles in which breakdown of the oocyte, zona pellucida and granulosa cells occurs. OVARIAN HORMONES Hypothalamic gonadotropin releasing factors (GnRH) stimulate secretion of pituitary basophil secretion of FSH early in the cycle and LH at the midpoint. FSH promotes follicular development and the LH surge causes ovulation and maintains the corpus luteum. Estrogen from ovarian follicles can stimulate (+) hypothalamic production of LHRH and inhibit (-) secretion of the releasing hormone for FSH. Progesterone and estrogen from the corpus luteum inhibit (-) releasing factor secretions from the hypothalamus. Hormone Source Gonadotropinreleasing hormone Function Stimulates release of FSH and LH from anterior pituitary Hypothalamus (GnRH) Prolactin-inhibiting Inhibits prolactin release by pituitary Acidophil factor Hypothalamus Follicle-stimulating Basophils of hormone anterior Stimulates secretion of estrogen and development of ovarian follicles (from secondary follicle onward) pituitary Luteinizing Basophils of Stimulates formation of estrogen and progesterone; hormone (LH) anterior promotes ovulation and formation of corpus luteum pituitary Estrogens Granulosa Inhibits release of FSH and GnRH; triggers surge of LH; cells of the causes proliferation and hypertrophy of myometrium of ovary uterus; causes development offemale sexual granulosa- characteristics, including breasts and body fat lutein cells of the corpus luteum; and placenta Progesterone Granulosa Inhibits the release of GnRH from the hypothalamus cells of the theca-lutein and ovary; LH from the basophils of the anterior pituitary; granulosa- causes the development of the uterine endometrium and lutein cells of regulates the viscosity of mucus produced by the glands the corpus of the uterine cervix; causes development of female luteum; and sexual characteristics including breasts placenta Inhibin Granulosa Inhibits FSH secretion by basophils of the anterior cells of the pituitary and ovary; granulosalutein cells Activin Granulosa Stimulates FSH secretion cells of the ovary Human chorionic Placenta gonadotropin(hCG) Human placental promotes the release of progesterone Placenta lactogen Relaxin Assists in the maintenance of the corpus luteum; Promotes mammary gland development during pregnancy; promotes lactogenesis Placenta Facilitates parturition by softening the fibrocartilage of the pubic symphysis; softens the cervix and facilitates its dilation in preparation for parturition Oxytocin Hypothalamus Stimulates smooth muscle contraction of the uterus via the during orgasm and during parturition; stimulates posterior contraction of myoepithelial cells of the mammary pituitary gland assisting in milk ejection Polycystic Ovarian Syndrome A disorder in which the ovaries are bilaterally enlarged with multiple follicular cysts due to abnormal regulation of the hypothalamic-pituitary-ovarian axis. Symptoms include amenorrhea, menstrual abnormalities, infertility, and hirsutism. Polycystic Ovaries develop when the ovaries are stimulated to produce excessive amounts of male hormones (androgens), particularly testosterone, either through the release of excessive luteinizing hormone (LH) by the anterior pituitary gland or through high levels of insulin in the blood (hyperinsulinaemia) in women whose ovaries are sensitive to this stimulus. This syndrome acquired its most widely used name because a common sign is multiple (poly) ovarian cysts. These form where egg follicles matured but were never released from the ovary because of abnormal hormone levels. OVIDUCT The oviducts are a pair of fibromuscular tubes that extend from the ovary to the uterus. Regions near the ovary have a well-developed mucosa while those near the uterus have a thick muscular wall. The oviduct which is also called the uterine or Fallopian tube conducts ova expelled from the ovary to the uterus. The oviduct has four distinct segments. The area closest to the ovary has a funnel shaped opening and is known as the infundibulum. The next region, the ampulla, is the longest segment and leads to a short isthmus which is adjacent to the uterus. The last segment of the oviduct is embedded in the wall of the uterus and is the intramural or uterine portion of the tube. Each one of these segments has a histology which is slightly different from the other. The mucosa of the oviduct is thrown in to longitudinal folds which is exaggerated in infundibulum and ampulla. They divide the lumen into labyrinthine spaces. The inner circular and outer longitudinal bands of smooth muscle in the oviduct serve to move the ovum toward the uterus. OVIDUCT CELLS Two distinct types of cells occupy the mucosa: ciliated simple columnar epithelial cells and secretory cells. The latter are wedged in between the ciliated cells and as a result are also called peg cells. They are nonciliated and produce a fluid that provides nutritive material for ovum. The ciliated cells keep the fluids secreted by the peg cells in motion . Research suggests that both ciliary movements and peristaltic muscular activity are involved in the movement of the oocyte. UTERUS A muscular organ which functions to provide a protective and nutritive environment for the developing fetus. It is made up of three parts Fundus , body and cervix. The wall of the uterus is made of three layers; the outer perimetiurm lined by serosa or adventitia; a thick smooth muscle layer called myometrium; and an inner endometrium. The myometrium is composed of interlacing bands of smooth muscle fibers which contract under the influence of oxytocin at parturition. They undergo Hyperplasia and hypertrophy during pregnancy. Uterine fibroids (also called leiomyomas or myomas) are benign growths of the muscle inside the uterus. They are not cancerous, nor are they related to cancer. Fibroids can cause a wide variety of symptoms, including heavy menstrual bleeding and pressure on the pelvis. About 25% of women in their reproductive years have noticeable fibroids. Part of the endometrium is lost in the menstrual flow and is rebuilt during each cycle. The endometrium is divided into functional (decidua functionalis) and basal (decidua basalis) regions. The functional area changes dramatically during the course of each cycle and is lost if pregnancy does not occur. The basal portion is close to the myometrium and is retained during menstruation to serve as stem cells for the functionalis during the next cycle. PROLIFERATIVE STAGE: The morphology of the endometrium changes during the menstrual cycle. It increases in height during the first part of the ovarian cycle, is maintained for a while and then is reduced to a basal level if the ovum is not fertilized. There are three stages of endometrial cycling. Following the cessation of menstruation, the endometrium goes through a proliferative phase in which glands and blood vessels increase in size, and this occurs under the influence of estrogen from the ovary. Under the influence of ovarian estrogen, the uterine endometrium lengthens during the proliferative stage of uterine development. Uterine tissues, both glandular and stromal tissues, proliferate. During this stage the glands are relatively straight and have the same type of simple columnar epithelial tissue as that at the surface. In the epithelium of a uterine gland, these nonciliated simple columnar epithelial cells accumlate glycogen. Blood vessels called spiral arteries lengthen and coil slightly. SECRETORY STAGE During the next phase, the secretory phase, the endometrium attains its greatest height and is capable of supporting the fetus should fertilization and implantation occur. Progesterone from the corpus luteum main-tains the endometrium. Should fertilization not occur, much of the endometrium is lost in the menstrual phase and is reduced to a small area near the myometrium. The secretory phase of the uterus commences with ovulation. During the secretory phase, both the spiral arteries and endometrial glands continue their development as the endometrium elongates. Under the influence of progesterone from the corpus luteum, the endometrium prepares itself to receive the fertilized ovum. It is during this phase that the endometrium is tallest in anticipation of a potential implantation. The surface columnar epithelium present in the proliferative stage persists. Endometrial glands become cork-screw in shape, and the lining cells secrete nutrients, especially glycogen, into the lumen. This dilates the glandular lumen. Spiral arteries continue to lengthen, become coiled and extend almost to the surface. MENSTRUAL STAGE In the menstrual phase of the uterine cycle, the stroma has become engorged with blood. The walls of the blood vessels become leaky and the glandular epithelium degenerates. The entire functionalis is lost during menstruation, and only the basal layer of the endometrium persists as a small area of tissue adjacent to the myometrium. The uterine stromal tissue indicates the presence of erythrocytes and there is accumulation of leukocytes in the lumens of the glands. CERVIX The neck of the uterus or cervix extends into the vaginal canal. The portion of the cervix extending into the vagina and lined by stratified squamous non keratinized epithelium is the called the ectocervix. Mucous membrane lining the cervical canal and the region of the opening of the cervical canal into the uterine cavity is called the endocervix. The wall of the cervix contains dense connective tissue and relatively little smooth muscle as compared to the uterus. Mucus secreting glands are located in the irregular outlines of the mucosa. Ducts from these glands can become occluded, and, as a result, the mucus dilates the lumen of the gland to form cysts ( Nabothian cysts). The cervix protects the uterus from bacterial infections and dilates during parturition to permit passage of the fetus. The cervical mucosa is lined by stratified squamous epithelium at its opening into the vagina, the porto vaginalis, and by simple columnar epithelium near its junction with the uterus proper, the ostium of the cervix. The columnar epithelium is not lost during menstruation. Cervical mucus exhibits changes in viscosity during the menstrual cycle. In the uterine proliferative phase, estrogen promotes the secretion of watery mucus which allows passage of spermatozoa into the uterus. After ovulation, the mucus secretions are more viscous to prevent the spread of bacteria. The squamous epithelial cells of the cervix are constantly being shed into the vagina. Specially stained preparations of these cells form the basis of Papanicolaou (pap) smears which can be used to diagnose the state of health of the cervix and can determine the presence of cervical carcinoma. The Transformation Zone (T zone) is located between the original squamo-columnar junction and the junction between the newly formed squamous metaplastic epithelium and the endocervical columnar epithelium. All cervical precancerous lesions develop from this zone. Invasive carcinoma of cervix: Malignant cells breach the basement membrane and invade local tissues and then to distant places. VAGINA The vagina is a fibromuscular canal extending from the cervix to the vestibule of the external genital organs is lined with stratified squamous epithelium that is not keratinized. Under the base-ment membrane of the epithelium is a lamina propria of connective tissue which is densely fibrous near the epithelium and becomes less dense near the smooth muscle. Elastic fibers are located just under the epithelium. The vagina does not contain glands. The wall of the organ is formed primarily of smooth muscle which is arranged in two indistinct layers consisting of inner circular and outer longitudinal coats. Striated muscle fibers may be present at the opening of the vagina at the vestibule. An adventitia of dense connective tissue lies outside of the muscle layers. During the follicular phase of the menstrual cycle, the epithelial cells of the vagina store glycogen. The glycogen is washed out of the cells in the preparative procedures for light microscopy, and as a result the outer layers of cells appear pale with small darkly stained nuclei. MAMMARY GLANDS Compound tubuloalveolar glands that lie in the superficial connective tissue of the thorax. Glandular elements are arranged in a radial fashion around the nipple into which ducts from the secretory units empty. Mammary gland histology varies with age and the physiological state of the individual. They attain their greatest morphological and functional development near the end of pregnancy and during the period of lactation. Their structure and function are affected by a variety of hormones from the ovary, placenta and pituitary. The epithelial cells in the alveoli in the nonpregnant individual are considered as elements of the duct system. Upon pregnancy these cells proliferate and, in the late stages prior to delivery of the fetus, become secretory. The ducts are lined by cuboidal or columnar cells and subtle changes in the ducts occur during the ovarian cycle. Early in the cycle the ducts appear as flattened cords of cells. Under the influence of estrogen, definitive lumens appear in the ducts and the potential secretory cells elongate. INACTIVE GLAND In inactive mammary glands, little, if any, secretions are produced by the alveolar cells. The flattened nuclei of fibroblasts are found in the connective tissue between the alveoli. PROLIFERATING GLAND As a result of the influence of estrogen and progesterone from the corpus luteum and placenta, the duct cells and secretory cells proliferate. Growth and development of the mammary glands during pregnancy are also dependent on prolactin which is produced by the anterior pituitary, by human placental lactogen (somatomammotropin), by adrenocorticoids and thyroid hormone. During the proliferative phase of breast development, the expanding epithelial secretory units fill the connective tissue between other units. The connective tissue within the secretory cluster exhibits an increase in cellularity from the infiltration of lymphocytes and proliferation of other cells. The developing secretory cells are arranged in two layers as a stratified cuboidal epithelium around a central lumen forming what will become, in the active gland, the alveoli. As pregnancy progresses, proliferation of secretory alveoli and duct cells continues at the expense of the connective tissue in the breast. Alveoli lined by cuboidal cells enlarge and begin secreting a protein-rich material called colostrum which expands the alveolar lumen. Colostrum accumulates in the lumen of the glands and ducts and is the first secretion of the mammary glands provided to the newborn. The presence of antibodies, especially immunoglobulin A (IgA), from the mother imparts a passive immunity to the infant. During pregnancy the increased numbers of alveoli displace the connective tissue between the secretory elements. LACTATING GLAND The morphology of the lactating gland is slightly different from the images of the gland in late pregnancy. As the result of the influence of prolactin from the adenohypophysis, the alveolar cells secrete milk proteins and other nutrients and proteins, especially immunoglobulin A (IgA), into the expanded alveoli which compress the secretory cells somewhat. The lactating gland appears morphologically similar to the thyroid or the lung because of this activity. The presence of a well developed system of ducts allows the lactating mammary gland to be distinguished from either of these two organs. Ducts and glands attain their greatest development during the last stages of pregnancy. The lumen of the glands is filled with their secretions. The myoepithelial cells of the lactating gland are stimulated to contract by oxytocin released from the neurohypophysis in response to suckling. Contractions of myoepithelial cells force milk from the alveoli into the duct system. Prolactin secretion and milk production continue as long as the child suckles. Weaning from the breast results in regression of breast tissue and resumption of the ovarian cycle which was suppressed by the process. The ducts of the mammary gland merge into fifteen to twenty lactiferous ducts that open at the nipple. The ducts are surrounded by dense connective tissue under the stratified squamous epithelium at the surface. Sebaceous glands, without associated hair follicles, are located in the dermis just below the epithelium. The glands open either onto the surface or into ducts. Their secretions lubricate the nipple during suckling. Free nerve endings and touch receptors (Meissner's corpuscles) are found in the dermal papillae. NONINVASIVE INTRADUCTAL CARCINOMA OF THE BREAST: Tumors, both benign and malignant neoplasms, constitute the majority of clinical disorders of the breast. Tumors can arise from a variety of sources, from epithelial tissue, glandular and ductal tissue, fibrous connective tissue and adipose tissue. The list of potential diseases extends from benign lipomas and fibromas to invasive and noninvasive carcinomas. Carcinoma of the breast is responsible for 20% of all the deaths by cancer of women. There are two major classes of breast cancer, noninvasive carcinomas and invasive or infiltrating carcinomas; each has several subclasses. Noninvasive intraductal carcinoma, constitutes about 20-30% of all breast cancers. It is characterized by the spread of malignant cells in the duct system. These cancer cells do not have the ability to cross the ducts’ basement membrane and do not metastasize. Vacuoles are in the epithelium and tumor cell clusters. PLACENTA The placenta functions in the exchange of material between the fetus and the mother and in the secretion of hormones important for the maintenance of pregnancy and the developing fetus. It is made up of two parts, the fetal part and the maternal part. The maternal part of the placenta is the decidua basalis of the endometrium containing anchoring villi, large decidual cells and a typical connective tissue stroma. The decidua basalis also conatins basal portions of uterine glands. The amniotic surface is lined by simple squamous cells deep to which is the connective tissue of the chorion. Deep to the connective tissue layer are the trophoblast cells of the chorion. The trophob;ast and the umderlying connective tissue form the chorionic plate. The anchoring villi arise from the chorionic plate, extend to the uterine wall and attach to the decidua basalis. Floating villi extend from the anchoring villi and float in the intervillous space which is bathed with maternal blood. DECIDUAL CELLS Following implantation, the cells of the uterine stroma enlarge and proliferate to form the bulk of the endometrial tissue. These are decidual cells and have pale staining nuclei with one or more nucleoli. Their cytoplasm contains numerous mitochondria and areas of rough endoplasmic reticulum. They provide nutrients to the developing embryo and secrete a hormone similar to pituitary prolactin which helps maintain the corpus luteum. CHORIONIC VILLUS Each chorionic villus has an outer syncytiotrophoblast layer of basophilic cells which have a brush border of microvilli at their surface to increase the absorptive area. The syncytiotrophoblastic cells secrete human chorionic gonadotrophin which maintains the corpus luteum of pregnancy following the decrease in luteinizing hormone secretion from the pituitary. In addition, syncytiotrophoblasts produce human chorionic lactogenic hormone which may aid in the stimulation of milk production in the mammary gland. Syncytiotrophoblastic cells secrete progesterone and estrogen as well. Each villus has a basal lamina which separates the epithelium from the subjacent core of loose connective tissue. Within the connective tissue core of the villi are branches of the umbilical arteries and vein. Fibroblasts and phagocytic cells (Hofbauer's cells) are also found there. The spaces between the villi are bathed by maternal blood. Nutrients are removed from the blood and wastes are excreted into the maternal blood. Immediately below the syncytio-trophoblast layer are the cyto-trophoblast cells which are abundant in the early stages of pregnancy. In the placenta at term the number of cells in this layer is greatly reduced. The cytotrophoblastic cells most likely serve as a stem cell population for the syncytiotrophoblastic cells. UMBILICAL CORD conducts vessels to and from the developing fetus, brings nutrients to the child and carries waste products away. The cord is lined with simple cuboidal epithelium similar to that of the amnion. Beneath the epithelium is mucous connective tissue containing fibroblasts, collagen fibrils and a gel-like matrix called Wharton's jelly. The umbilical cord has two arteries and one vein. The arteries convey wastes away from the fetus, and the veins bring nutrients and other materials to the fetus. The gel-like consistence of the mucous connective tissue imparts flexibility to the umbilical cord. Elongated fibroblasts and collagen fibrils form the bulk of the cord matrix. H I S T O L O G Y L A B O R A T O R Y Female Reproductive System OBJECTIVES: At the completion of this section, the student will be able to: Identify the tissues of the ovary, and distinguish between primordial, primary, secondary, tertiary and atretic follicles. Describe the three layers of the uterine tube and compare the structure in the different regions along its length. Describe the three layers of the uterus. Understand the morphological changes in the endometrium and myometrium during the normal menstrual cycle and during pregnancy. Compare the structures and functions of the mammary gland at different stages. Identify the three layers of the cervix and the vagina. Identify the villi and intervillous space in the placenta. Relate these structures with placental function. Laboratory Experience The purpose of this laboratory exercise is to identify the different tissues and cells found in the female reproductive system. Identify the cell types present and the tissue structure in each of the different organs. Use the slides listed below along with your manual, your text and your atlas to identify the cells, tissues and organs described. Ovary (#87) and Corpus Luteum (#88): Scan the section at low magnification. At the periphery, the ovary is lined by a simple cuboidal mesothelium, the germinal epithelium. Beneath the mesothelium is a layer of fibrous tissue, the tunica albuginea. Underlying the tunica albuginea is the less fibrous stroma and scattered within it are ovarian follicles. These structures constitute the ovarian cortex. In the center of the ovary is the medulla composed of loose connective tissue with large blood vessels and lymphatics. Ovarian follicles (found only in the cortex) are composed of an oocyte encircled by epithelia-like follicular (granulosa) cells. Be aware that all follicles are not cut through the center, many sections just graze the surfaces of follicles so that their stages may be difficult to distinguish. Borrow slides if necessary to see each of the following follicular stages: 1) Primordial follicles consist of flat follicular cells surrounding a primary oocyte. 2) Primary follicles have one or more layers of cuboidal follicular cells surrounding a primary oocyte. A thin zona pellucida lies between the oocyte and the follicular cells. 3) Secondary (antral) follicles have a thick granulosa (follicle cell layer) and a zona pellucida. They are distinguished by an antrum filled with liquor folliculi. The hillock of follicle cells that attach the oocyte to the follicle wall is called the cumulus oophorus. Around the periphery of the follicle are stroma cells which comprise the theca interna. The flattened spindle-shaped cells of the theca externa may also be apparent. This layer can be less distinctly visible. 4) Tertiary (Graafian / mature) follicles have a large antrum, and a thin granulosa layer. The mound-like cumulus oophorus will attach the zona pellucida-encapsulated oocyte to the follicle wall. Follicle cells that form a ring around the surface of the oocyte are called the corona radiata. Both layers of the theca are much more evident. 5) Atretic follicles are degenerating follicles and may arise during any developmental stage. The corpus luteum is a large group of yellowish cells from the wall of a tertiary follicle after the oocyte is ovulated. It is comprised mainly of granulosa lutein cells derived from the granulosa of the follicle and a smaller layer of theca lutein cells derived from the former theca interna. It serves as a temporary endocrine gland which persists for about 2 weeks. If fertilization and implantation occurs, it persists for several months. The corpus albicans is white, fibrous scar tissue that remains in the ovary after the corpus luteum has degenerated. Identify and check-off each of the following: ( ) Germinal epithelium ( ) Primordial follicle ( ) Tertiary follicle ( ) Zona pellucida ( ) Corpus albicans ( ) Tunica albuginea ( ) Cortex ( ) Medulla ( ) Primary follicle ( ) Secondary follicle ( ) Granulosa cell ( ) Theca Interna ( ) Antrum ( ) Cumulus oophorus ( ) Corpus luteum Uterine (Fallopian) Tube / Oviduct (#86): The proximal end of the uterine tube is near the ovary, where it opens and displays finger-like processes called fimbriae. The tube is loosely subdivided into 4 zones: the infundibulum with fimbriae nearest the opening; the ampulla (a short, thin-walled section); the longest segment, the isthmus which narrows into the intramural portion within the muscular wall of the uterus. All of the regions have the same layers, but proximally the mucosa is more highly folded than distally. Proximally the simple columnar epithelium contains more ciliated cells than Peg cells; distally, this ratio is reversed. Peg cells secrete a serous fluid into the lumen. Ciliated cells create currents that facilitate egg and sperm transport. The lamina propria is well vascularized and may contain lymphocytes. Beneath the lamina propria is the muscularis. The inner layer is primarily circular smooth muscle and the outer layer is primarily longitudinal. The serosa is vascular loose connective tissue covered by a simple squamous mesothelium. Examine the slide at low magnification; compare the mucosa with regard to diameter and number of folds. At high magnification, compare the number of ciliated versus secretory cells in the epithelium. Examine the lamina propria and the muscularis. Identify and check-off the following: ( ) Mucosa ( ) Lamina propria ( ) Smooth muscle / muscularis ( )Secretory peg cells ( ) Ciliated cells Uterus (#90): The wall of the uterus has 3 structurally and functionally distinct layers: 1) Perimetrium is the outermost layer composed of dense irregular connective tissue. 2) Myometrium is the middle and thickest layer comprised of interwoven layers of smooth muscle. Cyclic changes in cell numbers and size are mediated by the estrogen / progesterone balance. The myometrium is responsible for muscular support and for uterine contractions during partruition. 3) Endometrium is analogous to the mucosa and is lined by simple columnar epithelium with many ciliated cells and simple tubular glands rich in mucus secreting cells. The epithelium is underlain by a lamina propria. The endometrium is divided into a basal layer adjacent to the myometrium and a functional layer. The functional layer varies in thickness with stages of the menstrual cycle and is sloughed off during menstruation. Large blood vessels supply the uterus. Branches called straight arteries supply the basal layer of the endometrium and these branch to form spiral arteries which supply the functional layer. Spiral arteries constrict when progesterone / estrogen levels drop prior to menstruation. This results in lack of blood flow and leads to ischemia and shedding of the functional layer during menstruation. Both the uterus, and its stage in the menstrual cycle are identified by examining the endometrium. The proliferative phase has a relatively thin endometrium with short, straight glands. The secretory phase is characterized by a thick endometrium with noticeably elongated, widened, and coiled glands. Secretions may be visible in the uterine lumen and in the apical vacuoles of epithelial cells. The menstrual phase is characterized by stagnant pools of blood in distended vessels. Identify and check-off each of the following: ( ) Endometrium ( ) Basal layer ( ) Uterine glands ( ) Myometrium ( ) Perimetrium ( ) Lamina propria ( ) Functional layer ( ) Simple columnar epithelium ( ) Proliferative stage ( ) Secretory stage Cervix: Although no slides of the cervix exist in your slide box, you should be familiar with the histology of the cervix. Examine your text and atlas for information on the cervix. The narrow end of the uterus projects into the vagina and forms the short, tubular cervix. As it projects into the vagina, the cervical mucosa changes from a simple columnar epithelium to a stratified squamous epithelium. The glands in this region are called cervical glands; they secrete mucus whose consistency changes throughout the menstrual cycle. Estrogen stimulates production of a thick and viscous secretion which restricts entry of pathogens to the uterus. At ovulation, the secretions become watery to facilitate sperm entry. Progesterone stimulates production of a thick mucus that creates a cervical plug. Also under influence of estrogen, the cervix swells, exposing the uterine epithelium near the os of the cervical canal to the vaginal environment. This results in localized metaplasia; the columnar epithelium becomes squamous and monthly metaplasia may produce transformed cells which seed cervical cancer. Pap smears are made from cell scrapings taken from the area and are used to diagnose potentially cancerous cells. Early detection and treatment effectively reduces mortality rates for cervical and uterine cancer. Identify and check-off each of the following: ( ) Vaginal stratified squamous epithelium ( ) Uterine simple columnar epithelium ( ) Vaginal / uterine epithelial transition zone ( ) Cervical glands Vagina (#85): Scan the slide at low magnification and identify the mucosa which consists of a nonkeratinized, stratified squamous epithelium underlain by a thick, fibroelastic lamina propria containing lymphocytes. The relatively thick epithelium is interdigitated with tongues of lamina propria, an organization that increases surface adhesion. As the epithelial cells mature, they approach the surface, become vacuolated and release glycogen. The glycogen is converted into lactic acid by resident bacteria producing an acidic lumenal space. Flattened surface cells continuously detach from the apical surface and are seen in vaginal smears. Beneath the lamina propria is the muscularis which contains bundles of smooth muscle interwoven with a dense, fibrous matrix of connective tissue that is continuous with the adventitia. Identify and check-off each of the following: ( ) Mucosa ( ) Epithelium ( ) Lamina propria ( ) Muscularis Placenta (#89): As the zygote implants in the endometrium, its trophoblast cells proliferate and the placenta becomes a syncytium of placental villi interdigitated with the intervillous space containing maternal blood (supplied by the spiral arteries of the uterus). The placental villi project into the intervillous space and facilitate waste and nutrient exchange between the embryo and the mother. The villi contain a core of connective tissue overlain by cytotrophoblast cells. Some villi form large trunks which serve as a base for the smaller, more numerous villi involved with exchange. Villi that penetrate the syncytium and bind directly to uterine tissue are called anchoring villi. Identify and check-off each of the following: ( ) Placental villi ( ) Intervillous space ( ) Cytotrophoblast cells Inactive (Quiescent) Mammary Gland (Breast) (#92): At low magnification, the section is primarily composed of dense irregular connective tissue, islands of inactive lactiferous ducts, clusters of unilocular adipose tissue, and blood vessels. Scattered throughout the field are islands of intralobular lactiferous ducts. These are within lobules and have few secretory or alveolar units. The intralobular ducts are lined by simple cuboidal epithelium, but the epithelium may look stratified due to the presence of myoepithelial cells along the basal aspect. Myoepithelial cell nuclei contain condensed chromatin, and are triangular compared to the pale, round nuclei of the cuboidal cells. They may be difficult to discern on your slide. Identify and check-off each of the following: ( ) Lactiferous ducts ( ) Adipose tissue ( ) Simple cuboidal epithelium ( ) Myoepithelial cells ( ) Dense irregular connective tissue Lactating Mammary Gland (Breast) (# 91): At low magnification, the epithelium of the ducts is readily distinguished from the connective tissue. Lobules and large intralobular lactiferous ducts are surrounded by connective tissue. Each lobule has numerous distended alveoli that have proliferated along the length of the intralobular duct that contain lipid, protein and polysaccharide secretion products in their lumens. Intralobular ducts are smaller branches of the lactiferous ducts. Secretory epithelial cells are relatively large, slightly basophilic and have a vacuolated cytoplasm. Plasma cells are may be seen in the vascular lamina propria within the lobules. Flattened myoepithelial cells can also be observed beneath the secretory cells. Identify and check-off each of the following: ( ) Secretory alveoli ( ) Myoepithelial cells ( ) Lactiferous ducts ( ) Secretory cells Study Questions: What is the function of myoepithelial cells? What mode(s) of secretion are used by the glandular tissue of the breast? List the order of development of ovarian follicles. What is the role of glycogen release in the vagina? List the two types of epithelia found at the cervico-vaginal junction. Which layer of the endometrium is lost during menstruation? Which of the ovarian follicles does not contain a zona pellucida? List the epithelia found in the oviducts, in the uterus, in the cervix and in the vagina. What is found in the intervillous space of the placenta? FEMALE REPRODUCTIVE SYSTEM WORKSHEET FILL IN THE BOXES Structure Ovary Primordial follicle Primary follicle Secondary (antral) follicle Tertiary (mature / Graffian) follicle Identifying features (relevant layers, epithelia, and / or unique components) Clinical relevance (tests, diseases, morphological changes) Structure Corpus luteum Corpus albicans Oviduct Uterus Cervix Vagina Mammary gland Identifying features (relevant layers, epithelia, and / or unique components) Clinical relevance (tests, diseases, morphological changes)