Microanatomy- Female Reproductive System
advertisement

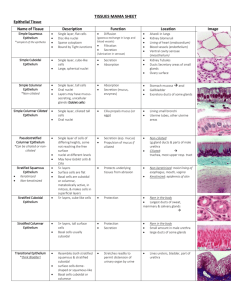
Female Reproductive Microanatomy Cat Ovaries: Two regions- cortex & medulla – only cortex is visible here due to sectioning Tunica Albuginea Germinal Epithelium Oocyte Follicular cells Primordial follicle- diagnostic feature is flattened follicular cells- shown above Primordial follicle development is under the control of activin- NOT FSH Secondary follicle- follicular cells become cuboidal in shape & lack of an antrum- subdivided into unilaminar and multilaminar Unilaminar follicle (surrounding cells are stromal cells of the CT) Multilaminar follicle basal lamina oocyte primordial zona pellucida Secondary Follicle antrum cumulus oophorus corona radiata Fully mature follicles reach the surface of the ovary- none do so in this slide Close-up of oocyte- blue ring is the zona pellucida composed of glycoproteins, surrounding this region is the cellular corona radiata Cells of the corona radiata are granulosar cells Secondary follicles are under FSH control Ovarian Medulla- diagnostic feature is arteries present Cortex medulla blood vessels Tunica Albuginea Antrum Germinal Epithelium Follicluar Cells Capillary Theca Interna Theca Externa Fimbrae infundibulum lumen of Fallopian Tube Simple Columnar epithelium of the fallopian tube epithelium 2 cell types present here- ciliated & peg cells- very difficult to differentiate in this image medulla cortex Corpus Luteum Diagnostic of corpus luteum are the folds present in the tissue- due to the follicular cells 2 cell types present in a Corpus luteum Granulosal luteal cells- large, foamy cells from granulosal layer (80%)- originally germinal epithelium derived Theca luteal cells- carried into the folds as they appear from the theca interna layer – secrete progesterone- originally stromally derived Granulosal luteal cells theca luteal cells Corpus Albicans- atretic corpus luteum infiltrated with fibroblasts forming a scar Note- if the epithelium is intact completely surrounding a space then it is probably a cyst and not a corpus albicans Fallopian Tube Cells: Simple Columnar epithelium Peg Cells Ciliated cells Uterus Functionalis layer Basalis layer Proliferative phase uterus- long thin glands w/ lots of CT between is diagnostic Coiled Helicine Arteries @ the base of the functionalis- diagnostic is a cluster of vessel lumens visible near the base of functionalis layer Straight capillaries are more difficult to find Gland of the functionalis layer- notice the simple columnar epithelium lining the glands Narrow lumen due to the proliferation phase Endometrium in secretory phase- larger lumens, dilated glands filled with glycogen, etc. substances Ragged cell borders will be seen due to constant secretion, also much less CT stroma between glands Caused by progesterone- causes secretion to occur (luteal phase) AKA progravida phase Proliferation/growth in proliferative phase is induced by estrogen secreted by the theca interna of the developing follicle Ovulation- LH Surge @ the end of the proliferative phase, caused by buildup of estrogen Estrogen is under negative feedback inhibition control via the pituitary (FSH secretion drops) Menstrual phase endometrium- most functionalis is gone Caused by smooth muscle cells of coiled arteries- loss of progesterone causes then to constrict, ischemia causes degeneration of vessels and eventually the sloughing occurs Cervix: Branched glandular ducts are diagnostic Strat. Squamous epithelium endocervical canal simple cuboidal epithelium Vaginal-cervical junction- transition pt from simple columnar to stratified squamous epithelium- weak point prone to chronic infection and subsequently cancer Important point for collection of pap smears Vagina- histological look alike to lower esophagus- epithelium both stratified squamous non-keratinized w/ few glands in esophagus and almost none in vagina MUST look at muscularis- esophagus is layered, vagina is mixed bundles Mammary Tissue Fatty Inactive tissue Glandular active tissue