RLF-05. Gastric-acce#1*S2#s

D’YOUVILLE COLLEGE
BIOLOGY 108/508 - HUMAN ANATOMY & PHYSIOLOGY II
LECTURE # 5
DIGESTIVE SYSTEM IV
STOMACH, PANCREAS, & LIVER
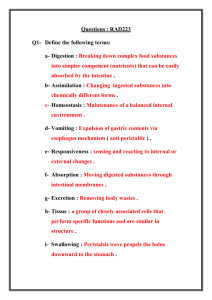
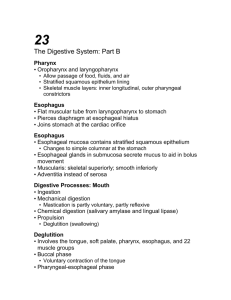
4. Abdominal Gastrointestinal Tract:
Stomach (fig. 23 – 14):
• J-shaped organ in left upper quadrant of abdominal cavity; lesser omentum suspends it by its lesser curvature from the liver; greater omentum extends inferiorly from its greater curvature
• fundus (above esophageal opening), body (spacious central part), pylorus
(antrum); pyloric valve at exit to duodenum
• muscularis has three layers instead of two (oblique (inner), circular and longitudinal (outer)), which provide mixing contractions (fig. 23 – 15)
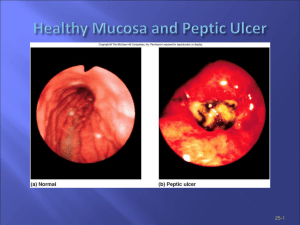
• mucosa (fig. 23 – 15): folded into rugae when the organ is empty; features tubular glands known as gastric pits or gastric glands) with three types of cell:
i. Neck (Mucus-secreting) Cells: lubrication and protection
ii. Parietal (Acid-secreting) Cells: hydrochloric acid denatures proteins, activates pepsin
iii. Chief (enzyme-secreting) Cells: pepsinogen (activated to pepsin by HCl) digests protein
- Other cells secrete intrinsic factor (required for absorption of vitamin B
12
) and several hormones, including gastrin (from endocrine cells)
• collective exocrine secretions of the gastric pits: mucus, water, hydrochloric acid, enzymes, & intrinsic factor comprise gastric juice
• neural and endocrine control of secretion (fig. 23 – 17):
i. Neural: parasympathetic fibers of vagus n. (cranial X) promote secretion of gastric juice and a hormone (gastrin)
ii. Endocrine: gastrin (from pylorus) extends gastric juice secretion; also certain food constituents (caffeine, spices, alcohol) known as “secretogogues” directly trigger gastric juice secretion
iii. Neural and Endocrine: entry of chyme into the duodenum triggers a
sympathetic nerve reflex (enterogastric reflex), which inhibits gastric secretion;
cholecystokinin (a hormone from duodenal mucosa) also inhibits further gastric secretion
• peristalsis moves small amounts of chyme into the pylorus; presence of chyme in pylorus triggers relaxation of pyloric valve - chyme enters duodenum
• different foods remain different times in stomach: carbohydrates and proteins remain for shorter periods; fats for 3 to 6 hours (longer satiety value)
• retrograde emptying (vomiting) - activation of a reflex from medulla
oblongata; also triggered by drugs (emetics), toxins, motion
Bio 108/508 lec. 5 - p. 2
Pancreas (figs. 23 – 21 & 23 – 26):
• mixed gland (exocrine & endocrine) posterior and inferior to the greater curvature of the stomach
• acini, (secretory units); pancreatic duct - joins the common bile duct (from liver) to form hepatopancreatic duct (empties into the duodenum)
• two types of secretion are produced:
a. Bicarbonate-rich Juice: neutralizes acidic chyme from the stomach; stimulated by an intestinal hormone, secretin
b. Enzyme-rich Juice: contains amylases, lipases, proteases (trypsin,
chymotrypsin, carboxypeptidase), and nucleases; proteases are activated in the intestinal lumen by enterokinase; another intestinal hormone, cholecystokinin, promotes this secretion (figs. 23 – 27 & 23 – 28)
Liver (fig. 23 – 21):
• largest organ of the abdominal cavity, occupies mainly the right upper
quadrant (right lobe); a small left lobe extends into left upper quadrant
•. Lobules (fig. 23 – 25): cylindrical columns of hepatocytes arranged in radial rows around a central vein - receive two distinct blood supplies: hepatic artery
(oxygen-rich blood) and hepatic portal vein (nutrient-rich blood from the small intestine); blood flows to the lobule’s central vein via spacious capillaries (sinusoids)
- drain via hepatic veins to inferior vena cava
• Metabolic Functions (figs. 24 – 13, 24 – 14, 24 – 15 & 24 – 16):
i. Carbohydrates: glucose oxidation: glycolysis, Krebs cycle & electron
transport system (aerobic); glycolysis only (anaerobic)
- glucose storage as glycogen (glycogenesis: stimulated by insulin); glucose release from glycogen (glycogenolysis: stimulated by glucagon)
- glucose production from non-carbohydrate sources, e.g. amino acid, fatty acid, (gluconeogenesis: stimulated by glucagon & cortisol)
ii. Lipids: triglycerides broken down to glycerol & fatty acids
• fatty acids oxidized for energy or reconstitute triglycerides
• triglycerides and cholesterol bound into lipoproteins: HDL: high protein content, LDL: low protein content, VLDL: very low protein content
• cholesterol synthesized (from acetyl-CoA) or excreted (via bile) according to the body’s need; cholesterol converted to bile salts (emulsifying agents)
iii. Proteins: essential amino acids (required in diet)
• nonessential amino acids formed from essential amino acids as required and secreted into bloodstream (amino acid pool)
• amino acids assembled into plasma proteins, e.g. lipoproteins
• amino acids oxidized by deamination; ammonia (produced by oxidations) is converted to urea via urea cycle
iv. Bile Formation and Secretion: bile contains cholesterol, water, bile salts, bile pigments (from hemoglobin), and other substances
• released in response to cholecystokinin (gall bladder contraction)
• substances (e.g. calcium, cholesterol) may come out of solution forming
gall stones (may cause obstruction of biliary tract)
Bio 108/508 lec. 5 - p. 3
Biliary System (fig. 23 – 25): hepatocytes secrete bile into tiny ducts
(canaliculi) - drained by hepatic ducts to common hepatic duct; bile may be passed to the gall bladder (for storage) via a cystic duct, or it may be delivered directly to the duodenum via the common bile duct