Questions
advertisement
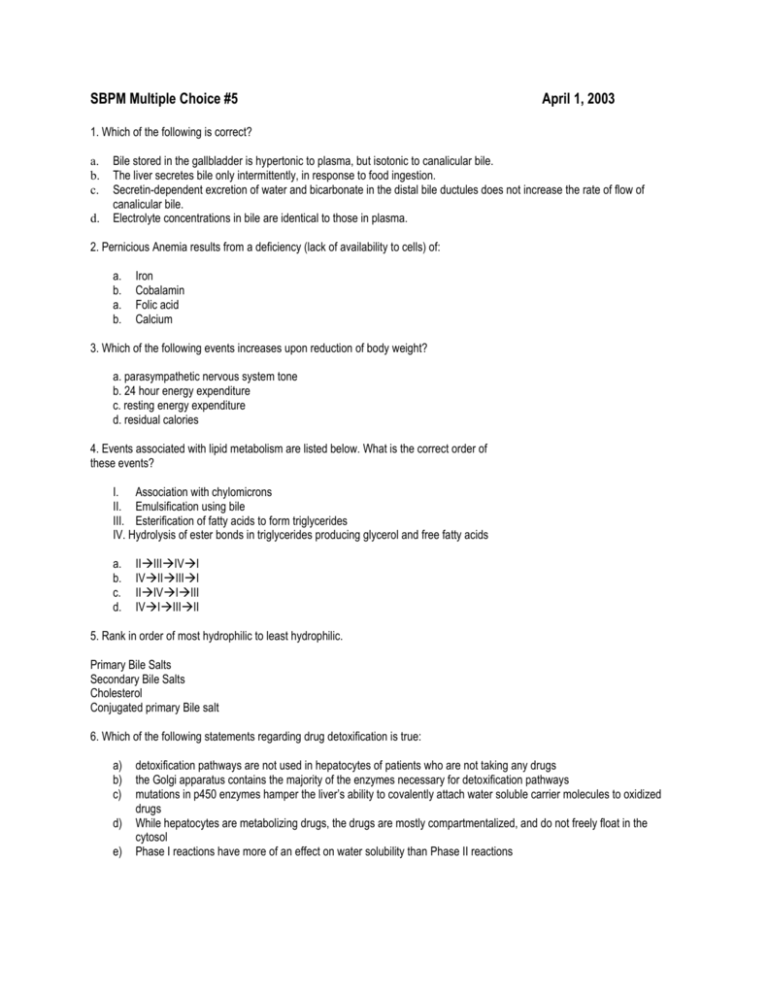
SBPM Multiple Choice #5 April 1, 2003 1. Which of the following is correct? a. b. c. d. Bile stored in the gallbladder is hypertonic to plasma, but isotonic to canalicular bile. The liver secretes bile only intermittently, in response to food ingestion. Secretin-dependent excretion of water and bicarbonate in the distal bile ductules does not increase the rate of flow of canalicular bile. Electrolyte concentrations in bile are identical to those in plasma. 2. Pernicious Anemia results from a deficiency (lack of availability to cells) of: a. b. a. b. Iron Cobalamin Folic acid Calcium 3. Which of the following events increases upon reduction of body weight? a. parasympathetic nervous system tone b. 24 hour energy expenditure c. resting energy expenditure d. residual calories 4. Events associated with lipid metabolism are listed below. What is the correct order of these events? I. Association with chylomicrons II. Emulsification using bile III. Esterification of fatty acids to form triglycerides IV. Hydrolysis of ester bonds in triglycerides producing glycerol and free fatty acids a. b. c. d. IIIIIIVI IVIIIIII IIIVIIII IVIIIIII 5. Rank in order of most hydrophilic to least hydrophilic. Primary Bile Salts Secondary Bile Salts Cholesterol Conjugated primary Bile salt 6. Which of the following statements regarding drug detoxification is true: a) b) c) d) e) detoxification pathways are not used in hepatocytes of patients who are not taking any drugs the Golgi apparatus contains the majority of the enzymes necessary for detoxification pathways mutations in p450 enzymes hamper the liver’s ability to covalently attach water soluble carrier molecules to oxidized drugs While hepatocytes are metabolizing drugs, the drugs are mostly compartmentalized, and do not freely float in the cytosol Phase I reactions have more of an effect on water solubility than Phase II reactions 7. The mechanism of excretion of K+ ingested from a person’s diet primarily involves a) b) c) d) decreased reabsorption of K+ by the proximal tubule and loop of Henle and increased secretion of K+ by the distal segments increased aldosterone secretion, increased secretion of K+ by the distal segments and increased urinary flow rate increased ADH secretion, increased secretion of K+ by the proximal segments and increased urinary flow rate increased aldosterone secretion and decreased reabsorption of K+ by the proximal tubule and loop of Henle 8. A patient presents in the ER with a BP of 90/60, dry mucous membranes and ABG values of pH 7.56, [HCO 3-] 50 mEq/L and pCO2 58 mm Hg, what type of acid-base abnormality is this and which of the following responses would you also expect to see in this patient? a) b) c) d) metabolic alkalosis, hyperventilation respiratory alkalosis, decreased K+ secretion by the distal tubules metabolic alkalosis, exchange of intracellular H+ for extracellular K+ respiratory alkalosis, increased ratio of H2PO4- to HPO4-2 in the urine 9. Which of the following associations is INCORRECT? a) b) c) d) cardiac arrhythmia --- hyperkalemia flaccid paralysis --- hypokalemia type 1 diabetes mellitus --- hyperkalemia β-blockers --- hypokalemia 10. Match the ENS transmitters with their functions a. 5HT3 b. 5HT1p c. 5HT4 ______activate myenteric IPAN with transmission to extrinsic sensory neurons ______activate submucosal IPAN ______enhance pre-synaptic release of submucosal IPAN vescicles 11. Match these drugs with their functions a. Ondansetron b. Tegaserod c. SSRI ______5-HT3 antagonist ______5-HT4 agonist ______ SERT inhibitor 12. What happens to patients with IBS patients who have SERT mutations that fail to recycle serotonin? a. b. c. d. diarrhea constipation alternative diarrhea and constipation bloody stool 13. Which of the following correctly describes the some of the body’s afferent and efferent responses to high sodium intake and volume expansion? A. High salt intake stimulates firing of the sympathetic nerves, which increases the amount of epinephrine and norepinephrine circulating. This allows vasodilatation, which increases the capacity of the circulatory system to accommodate the large ECV. B. Increased salt intake is sensed by osmoreceptors in the hypothalamus, which responds by increasing its synthesis and release of aldosterone, which tells the kidney to retain water. C. Increased ECV is sensed by volume receptors in the heart and carotid arteries, which causes inhibition of the sympathetic nervous system. In the absence of sympathetic stimulation, the kidney produces less renin, and consequently there is less Angiotensin II circulating and sodium reabsorption decreases. D. Volume receptors sense an increase in ECV and provoke the release of antidiuretic hormone (ADH) from the adrenal cortex, causing the collecting duct to become more permeable to NaCl, thus allowing more to be excreted. E. Volume receptors in the left atrium cause release of atrial natriuretic peptide (ANP) from myocytes, which decreases GFR by constricting the afferent arteriole. 14.When compared to normal steady state, what effect would severe dehydration have on the relationship between plasma osmolality and plasma [ADH]? A. B. C. D. E. Lower set point, shallower curve Lower set point, steeper curve Higher set point, shallower curve Higher set point steeper curve No change 15. Which one of the following is NOT part of the glomerular filtration barrier? a. Capillary endothelial cells b. Type IV collagen c. Podocytes d. Mesangial cells 16. The concentration of creatinine in a patient's plasma is 0.6 mg/ml. You collect the urine produced by the patient over 24 hours (1.2L) and find that the concentration of creatinine in the urine is 70 mg/ml. What is the patient's GFR? a. 68 ml/min b. .007 ml/min c. 97 ml/min d. 140 ml/min 17. Which of the following is not true? a) secretin is the main stimulus for bicarb secretion in the pancreas b) hyperosmolarity is a stimulus to secretion c) digestive enzymes are released in a fixed ratio upon stimulation d) acetylcholine directly causes the release of secretin 18. Which of the following is not part of GIP's action? a) inhibition of gastrin stimulated secretion b) inhibition of gastric motility c) stimulation of insulin release d) acceleration of gastric emptying time