Physiology of the Digestive System
advertisement
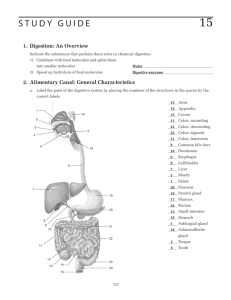
Physiology of the Digestive System Chapter 26 Anatomy & Physiology Mechanical Digestion • Consists of all motility that brings about: – Change in physical state of food from large to small – Churning – Propelling food forward Mastication (chewing) • Begins in mouth • Tongue, cheeks, lips keep food between the surfaces of teeth • Reduce particle size & mix with saliva Deglutition •Oral stage: mouth to oropharynx (voluntary control); under control of cerebral cortex •Pharyngeal stage: oropharynx to esophagus (involuntary); deglutition center in medulla •Esophageal stage: esophagus to stomach (involuntary); deglutition center in medulla Oral stage • Bolus in the middle of tongue pressed against the palate & moved back into the oropharynx • Soft palate & uvula prevent food from entering nasopharynx Pharyngeal stage • Involuntary reflexes push bolus toward esophagus • Upward movement of larynx & downward movement of food closes epiglottis Motility of smooth muscle in GI tract • Peristalsis • Segmentation Peristalsis •Wavelike ripple; always in a forward direction •Bolus stretching GI wall triggers a reflex contraction of circular muscle Segmentation •Mixing movement; forward & backward movement Gastric motility • Takes 2-6 hours to empty stomach • Food churned with gastric juices: chyme • Hormonal control: gastric inhibitory peptide secreted by intestinal mucosa • Nervous mechanism: triggered by presence of acid & distentionenterogastric reflex Intestinal motility • Both segmentation & peristalsis • Segmentation in duodenum & jejunum mixes chyme w/digestive juices • Takes 5 hours in small intestine • Peristalsis also stimulated by cholecystokinin-pancreozymin (CCK) secreted by intestinal mucosa in presence of chyme Digestive enzymes • Extracellular, protein catalysts • Enzyme principles – Specific in action – Function best a specific pH – Catalyze reaction in both directions – Continually being destroyed or eliminated so continually being synthesized – Most digestive enzymes are inactive proenzymes Carbohydrate digestion •Polysaccharides hydrolyzed by amylases (in saliva & pancreatic juices) to disaccharides •Sucrase, lactase, maltase found in cell membrane of villi cells hydrolyze into monosaccharides, mostly glucose Protein digestion •Proteases catalyze hydrolysis into intermediate compounds then finally into amino acids •Main proteases –Pepsin-stomach –Trypsin-pancreas –Chymotrypsin- “ –Peptidase-intestines Fat digestion •Lecithin & bile acids in bile emulsify (become small droplets soluble in water) fats •Main fat digesting enzyme: pancreatic lipases Residues of digestion • Cellulose: dietary fiber • Undigested connective tissue from meat Saliva • Secretion of salivary glands – Water (mostly) – Mucus: lubricates food – Salivary amylase: begins digestion of starches – Sodium bicarbonate: increases pH for optimal amylase activity Gastric juice • Secreted by gastric glands – Pepsin (by chief cells as pepsinogen)begins digestion of proteins – HCl (by parietal cells) decreases pH for activation & function of pepsin – Intrinsic factor (by parietal cells) protect vitamin B12 – Mucus & water Pancreatic juice • Secreted by acinar cells & duct cells – Proteases (trypsin & chymotrypsin) – Lipases – Nucleases: digest nucleic acids – Amylase – Sodium bicarbonate: increase pH • All pancreatic enzymes are secreted as inactive proenzymes Bile • Secreted by liver, stored & concentrated in gall bladder – Lecithin & bile salts – Sodium bicarbonate for optimum pH – Cholesterol, detoxification products, bile pigments all eliminated in feces Intestinal juice • Secreted by cells of intestinal exocrine cells – Mucus & water: lubricate & aid in mixing – Sodium bicarbonate Control of salivary secretions • Only by reflex mechanisms • Chemical, mechanical, olfactory, visual stimuli Control of gastric secretion •Three phases: –Cephalic phase –Gastric phase –Intestinal phase Cephalic phase • Activated by mental factors • Vagus nerve stimulates production of gastrin which stimulates gastric secretions Gastric phase • Products of protein digestion stimulate release of gastrin • Distension of stomach also stimulates release of gastrin Intestinal phase • Fats, carbohydrates & acid in chyme stimulate release of gastric inhibitory peptide (GIP), CCK, secretin which decrease gastric secretion Control of pancreatic secretion • Stimulated by hormones secreted by intestinal mucosa – Secretin: production of pancreatic fluid low in enzyme but high in bicarbonate – CCK • Increased exocrine secretion by pancreas • Opposes gastrin, thus inhibiting gastric secretion • Stimulates contraction of gallbladder Absorption • Passage of substances through the intestinal mucosa into blood • Most occurs in small intestines • Water: osmosis • Secondary active transport: sodium • Sodium cotransport: glucose • With the aid of bile salts in lacteals Elimination • Expulsion of the residues of digestion • Act of expelling feces is defecation • Defecation results as a reflex stimulated by receptors in rectal mucosa when rectum is distended



![Anti-GLP1 antibody [1B7B4] ab36598 Product datasheet 2 Images Overview](http://s2.studylib.net/store/data/011965712_1-746457d50999eb2b6a5b0653f270ecad-300x300.png)