Chapter 23 Part B - FacultyWeb Support Center
advertisement

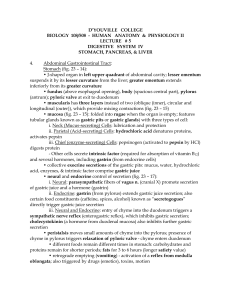
23 The Digestive System: Part B Pharynx • Oropharynx and laryngopharynx • Allow passage of food, fluids, and air • Stratified squamous epithelium lining • Skeletal muscle layers: inner longitudinal, outer pharyngeal constrictors Esophagus • Flat muscular tube from laryngopharynx to stomach • Pierces diaphragm at esophageal hiatus • Joins stomach at the cardiac orifice Esophagus • Esophageal mucosa contains stratified squamous epithelium • Changes to simple columnar at the stomach • Esophageal glands in submucosa secrete mucus to aid in bolus movement • Muscularis: skeletal superiorly; smooth inferiorly • Adventitia instead of serosa Digestive Processes: Mouth • Ingestion • Mechanical digestion • Mastication is partly voluntary, partly reflexive • Chemical digestion (salivary amylase and lingual lipase) • Propulsion • Deglutition (swallowing) Deglutition • Involves the tongue, soft palate, pharynx, esophagus, and 22 muscle groups • Buccal phase • Voluntary contraction of the tongue • Pharyngeal-esophageal phase • Involuntary • Control center in the medulla and lower pons Stomach: Gross Anatomy • Cardiac region (cardia) • Surrounds the cardiac orifice • Fundus • Dome-shaped region beneath the diaphragm • Body • Midportion Stomach: Gross Anatomy • Pyloric region: antrum, pyloric canal, and pylorus • Pylorus is continuous with the duodenum through the pyloric valve (sphincter) • Greater curvature • Convex lateral surface • Lesser curvature • Concave medial surface Stomach: Gross Anatomy • Lesser omentum • From the liver to the lesser curvature • Greater omentum • Drapes from greater curvature • Anterior to the small intestine Stomach: Gross Anatomy • ANS nerve supply • Sympathetic via splanchnic nerves and celiac plexus • Parasympathetic via vagus nerve • Blood supply • Celiac trunk • Veins of the hepatic portal system Stomach: Microscopic Anatomy • Four tunics • Muscularis and mucosa are modified • Muscularis externa • Three layers of smooth muscle • Inner oblique layer allows stomach to churn, mix, move, and physically break down food Stomach: Microscopic Anatomy • Mucosa • Simple columnar epithelium composed of mucous cells • Layer of mucus traps bicarbonate-rich fluid beneath it • Gastric pits lead into gastric glands Gastric Glands • Cell types • • • • Mucous neck cells (secrete thin, acidic mucus) Parietal cells Chief cells Enteroendocrine cells Gastric Gland Secretions • Glands in the fundus and body produce most of the gastric juice • Parietal cell secretions • HCl • pH 1.5–3.5 denatures protein in food, activates pepsin, and kills many bacteria • Intrinsic factor • Glycoprotein required for absorption of vitamin B12 in small intestine Gastric Gland Secretions • Chief cell secretions • Inactive enzyme pepsinogen • Activated to pepsin by HCl and by pepsin itself (a positive feedback mechanism) Gastric Gland Secretions • Enteroendocrine cells • Secrete chemical messengers into the lamina propria • Paracrines • Serotonin and histamine • Hormones • Somatostatin and gastrin Mucosal Barrier • Layer of bicarbonate-rich mucus • Tight junctions between epithelial cells • Damaged epithelial cells are quickly replaced by division of stem cells Homeostatic Imbalance • Gastritis: inflammation caused by anything that breaches the mucosal barrier • Peptic or gastric ulcers: erosion of the stomach wall • Most are caused by Helicobacter pylori bacteria Digestive Processes in the Stomach • Physical digestion • Denaturation of proteins • Enzymatic digestion of proteins by pepsin (and rennin in infants) • Secretes intrinsic factor required for absorption of vitamin B12 • Lack of intrinsic factor pernicious anemia • Delivers chyme to the small intestine Regulation of Gastric Secretion • Neural and hormonal mechanisms • Stimulatory and inhibitory events occur in three phases: 1. Cephalic (reflex) phase: few minutes prior to food entry 2. Gastric phase: 3–4 hours after food enters the stomach Regulation of Gastric Secretion 3. Intestinal phase: brief stimulatory effect as partially digested food enters the duodenum, followed by inhibitory effects (enterogastric reflex and enterogastrones) Regulation and Mechanism of HCl Secretion • Three chemicals (ACh, histamine, and gastrin) stimulate parietal cells through second-messenger systems • All three are necessary for maximum HCl secretion • Antihistamines block H2 receptors and decrease HCl release Response of the Stomach to Filling • Stretches to accommodate incoming food • Reflex-mediated receptive relaxation • Coordinated by the swallowing center of the brain stem • Gastric accommodation • Plasticity (stress-relaxation response) of smooth muscle Gastric Contractile Activity • Peristaltic waves move toward the pylorus at the rate of 3 per minute • Basic electrical rhythm (BER) initiated by pacemaker cells (cells of Cajal) • Distension and gastrin increase force of contraction Gastric Contractile Activity • Most vigorous near the pylorus • Chyme is either • Delivered in ~ 3 ml spurts to the duodenum, or • Forced backward into the stomach Regulation of Gastric Emptying • As chyme enters the duodenum • Receptors respond to stretch and chemical signals • Enterogastric reflex and enterogastrones inhibit gastric secretion and duodenal filling • Carbohydrate-rich chyme moves quickly through the duodenum • Fatty chyme remains in the duodenum 6 hours or more Small Intestine: Gross Anatomy • Major organ of digestion and absorption • 2–4 m long; from pyloric sphincter to ileocecal valve • Subdivisions 1. Duodenum (retroperitoneal) 2. Jejunum (attached posteriorly by mesentery) 3. Ileum (attached posteriorly by mesentery) Duodenum • The bile duct and main pancreatic duct • Join at the hepatopancreatic ampulla • Enter the duodenum at the major duodenal papilla • Are controlled by the hepatopancreatic sphincter Structural Modifications • Increase surface area of proximal part for nutrient absorption • Circular folds (plicae circulares) • Villi • Microvilli Structural Modifications • Circular folds • Permanent (~1 cm deep) • Force chyme to slowly spiral through lumen Structural Modifications • Villi • Motile fingerlike extensions (~1 mm high) of the mucosa • Villus epithelium • Simple columnar absorptive cells (enterocytes) • Goblet cells Structural Modifications • Microvilli • Projections (brush border) of absorptive cells • Bear brush border enzymes Intestinal Crypts • Intestinal crypt epithelium • Secretory cells that produce intestinal juice • Enteroendocrine cells • Intraepithelial lymphocytes (IELs) • Release cytokines that kill infected cells • Paneth cells • Secrete antimicrobial agents (defensins and lysozyme) • Stem cells Submucosa • Peyer’s patches protect distal part against bacteria • Duodenal (Brunner’s) glands of the duodenum secrete alkaline mucus Intestinal Juice • Secreted in response to distension or irritation of the mucosa • Slightly alkaline and isotonic with blood plasma • Largely water, enzyme-poor, but contains mucus • Facilitates transport and absorption of nutrients Liver • Largest gland in the body • Four lobes—right, left, caudate, and quadrate Liver • Falciform ligament • Separates the (larger) right and (smaller) left lobes • Suspends liver from the diaphragm and anterior abdominal wall • Round ligament (ligamentum teres) • Remnant of fetal umbilical vein along free edge of falciform ligament Liver: Associated Structures • Lesser omentum anchors liver to stomach • Hepatic artery and vein at the porta hepatis • Bile ducts • Common hepatic duct leaves the liver • Cystic duct connects to gallbladder • Bile duct formed by the union of the above two ducts Liver: Microscopic Anatomy • Liver lobules • Hexagonal structural and functional units • Filter and process nutrient-rich blood • Composed of plates of hepatocytes (liver cells) • Longitudinal central vein Liver: Microscopic Anatomy • Portal triad at each corner of lobule • Bile duct receives bile from bile canaliculi • Portal arteriole is a branch of the hepatic artery • Hepatic venule is a branch of the hepatic portal vein • Liver sinusoids are leaky capillaries between hepatic plates • Kupffer cells (hepatic macrophages) in liver sinusoids Liver: Microscopic Anatomy • Hepatocyte functions • Process bloodborne nutrients • Store fat-soluble vitamins • Perform detoxification • Produce ~900 ml bile per day Bile • Yellow-green, alkaline solution containing • Bile salts: cholesterol derivatives that function in fat emulsification and absorption • Bilirubin: pigment formed from heme • Cholesterol, neutral fats, phospholipids, and electrolytes Bile • Enterohepatic circulation • Recycles bile salts • Bile salts duodenum reabsorbed from ileum hepatic portal blood liver secreted into bile The Gallbladder • Thin-walled muscular sac on the ventral surface of the liver • Stores and concentrates bile by absorbing its water and ions • Releases bile via the cystic duct, which flows into the bile duct