Document

©2007 UpToDate ®
ACC/AHA guidelines on management of chronic heart failure: stages in the evolution of heart failure and recommended therapy by stage
Data from Hunt, SA, Abraham, WT, Chin, MH, et al. ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult. Circulation 2005; 112:e154.
DIABETIC KETOACIDOSIS
Def: severe insulin deficiency causes accumulation of B-hydroxybutyric and acetoacetic acid due to increased peripheral lipolysis and B-oxidation of those fatty acids in liver; these fatty acids are converted to ketone bodies; hyperglycemia with osmotic diuresis causes hypovolemia
Precipitants: infection, stress, MI, CVA, hypokalemia, renal failure, pancreatitis, dehydration, insulin deficiency, drugs (steroids, HCTZ, BB, dilantin, EtOH, CCB, cocaine)
Symptoms: polydipsia, polyphagia, weight loss, vomiting, abdominal pain, dehydration, weakness, clouding of sensorial, poor skin turgor, Kussmaul respirations, tachycardia, hypotension, alteration in mental status, shock, hypothermia, and ultimately coma.
Diagnosis: glucose >250 mg/dl, pH <7.35 or bicarb <18, + ketonuria or ketonemia
Initial labs: CBC, CMP, Mg, PO4, ABG, UA, serum ketones
Electrolyte: pseudohyponatremia —for every 100mg/dl glucose>150, add 1.6 to Na
K
—may initially be hyperkalemic but this is due to cellular shift as there is actually total body deficit from polyuria, vomiting, acidosis (true of phos as well)
ABG: anion gap metabolic acidosis +/- respiratory alkalosis
Serum Osmoles: serum osmolality >320 correlates with mental confusion
CBC: leukocytosis with left shift with or without infection
LFTs: amylase and lipase elevation, regardless if pancreatitis or peritonitis is present
Consider cardiac enzymes, drug screen, blood cultures, EKG, CXR, urine hcg
Mgmt: aggressive IVF hydration with insulin
Accucheck q1hr, BMP w/Mg and PO4 q2hrs until BS <250 then q4hrs until no anion gap
Begin dextrose containing IVF when BS <200, add K to IVF when K <5.3.
Gastric ulcer prophylaxis and anti-emetic, antibiotics if indicated
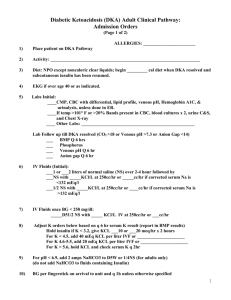
See orders/protocol for specific management
Initiate diabetic education, social services if needed for insulin needs, dietician if needed
HYPEROSMOLAR HYPEROSMOTIC STATE (HHS)
Symptoms : dehydration, mental status changes, SZ, CVA, hemiparesis, fever, thirst, polyuria, oliguria, hypotension, tachycardia, fever, usually slower onset than DKA, abd pain uncommon
Diagnosis: as above for DKA but generally glucose >600, pH normal, bicarb >15, anion gap
<12, normal to small serum and urine ketones, calculated osmolality likely >320
Mgmt: fluids as above but typically have 9L water deficit (greater than in DKA)
Diabetic Management in Hospital
Insulin requirements may increase with pain, trauma, surgery, sepsis, hypoxia, stress
Estimate total insulin requirements (0.6-1U/kg/day)
Give 50% as basal insulin (may overlap with insulin drip x1-2hrs), divide other 50% by number of meals per day and give as Novolog or regular insulin
2007 UpToDate Protocol for the management of adult patients with DKA
Phosphate: no benefit of phosphate replacement on the clinical outcome in DKA; however, in patients with cardiac dysfunction, anemia, or respiratory depression and in those with serum phosphate concentration <1.0 mg/dl, 20 to 30 mEq/l potassium phosphate can be added to replacement fluids.