L4_Diabetes Mellitus..
advertisement

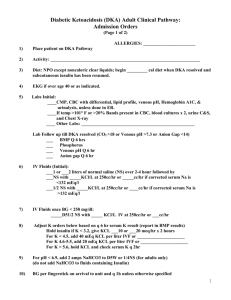
Diabetes Mellitus Ibrahim Sales, Pharm.D. Assistant Professor of Clinical Pharmacy King Saud University isales@ksu.edu.sa Hyperglycemic Crises in Diabetes • Diabetes ketoacidosis (DKA) and hyperosmolar hyperglycemic state (HHS) • Type 1 and Type 2 diabetes • Insulin deficiency and increased counterregulatory hormones leads to free fatty acids release and hepatic fatty acid oxidation to ketone bodies in DKA • Insulin concentrations inadequate for glucose uptake, but adequate to prevent ketogenesis in HHS Precipitating Factors • • • • • • • The most common is infection Cerebrovascular accident Alcohol abuse Pancreatitis Myocardial infarction Trauma Drugs (corticosteroids, thiazides, sympathomimetic agents) Signs and Symptoms • HHS evolves over several days to weeks • Symptoms of DKA may be present over several days; ketoacidosis-related metabolic alterations usually occur in < 24 hours • Polyuria, polydipsia, polyphagia, weight loss, vomiting, abdominal pain (DKA only), dehydration, weakness, clouding of sensoria • Poor skin turgor, Kussmaul respirations (DKA), tachycardia, hypotension, alteration in mental status, shock, coma (more frequent in HHS) Diagnosis Fluid Therapy • Goals: expansion of intravascular and extravascular volume and restoration of renal perfusion • 0.9% NaCl at the rate of 15-20mL/kg per hour or 1-1.5L during the first hour • Hypernatremic or eunatremic, 0.45% NaCl infused at 4-14mL/kg/hour • Hyponatremic, 0.9% NaCl infused at 414mL/kg/hour • Replace half of the estimated water deficit over a period of 12-24 hours Fluid Therapy • Patients with DKA and HHS require calories for proper metabolism of ketone bodies • DKA: When blood glucose falls below 200mg/dL, change to 5% dextrose with 0.45%NaCl at a rate of 150-250mL/hour • In HHS, When blood glucose falls between 200-250mg/dL, change to 5% dextrose with 0.45%NaCl at a rate of 150-250mL/hour Insulin Therapy • Potassium value should be >3.3mEq/L • IV bolus of regular insulin (0.1 units/kg body weight) • Continuous infusion of regular insulin (0.1 units/kg/hr) • Optimal rate of glucose reduction between 50-70 mg/hr • Decrease rate to 0.05 – 0.1 units/kg/hr when glucose reaches 200mg/dL (DKA); 300mg/dL (HHS) Insulin Therapy Blood should be drawn every 2–4 h for determination of serum electrolytes, glucose, blood urea nitrogen, creatinine, osmolality, and venous pH (for DKA). DKA • Criteria for resolution of DKA include: – Glucose 200 mg/dL – Serum bicarbonate 18 mEq/L – Venous pH 7.3 • Keep serum glucose between 150 and 200mg/dL until resolution HHS • Keep serum glucose between 250 and 300 until plasma osmolality is ≤315 mOsm/kg and patient is mentally alert Insulin Therapy • When the patient is able to eat, start a multiple-dose insulin schedule • Continue IV insulin for 1–2 h after the SQ insulin • Continue IV insulin in patients n.p.o. • Continue previous doses prior to admission in patients with known DM • Start a basal and bolus insulin schedule in insulin naïve patients (0.5-0.8 units/kg/day) Potassium • Hyperkalemia on presentation is common • Initiate K+ after serum levels <5.3mEq/L • 20–30 mEq K+ in each liter of infusion fluid to maintain a concentration between 4-5mEq/L • Hypokalemia: delay insulin until K+ is >3.3mEq/L Bicarbonate and Phosphate Bicarbonate • Insulin blocks lipolysis and resolves ketoacidosis without any added bicarbonate • Give 50 mmol of bicarbonate in 200 ml of sterile water with 10 mEq KCL over two hours to maintain the pH at > 7.0 in patients with pH between 6.9 and 7.0 Phosphate • Serum phosphate is often normal or increased at presentation • Phosphate concentration decreases with insulin therapy • When needed, 20 –30 mEq/L potassium phosphate can be added to replacement fluids Prevention of DKA and HHS • Prevention is the key (better access to medical care, proper education, effective communication with a health care provider during illness) • Sick-day management should include the following information: 1) 2) 3) 4) When to contact the health care provider Blood glucose goals and the use of supplemental short or rapid-acting insulin during illness Means to suppress fever and treat infection Initiation of an easily digestible liquid diet containing carbohydrates and salt • Advise all patients to never discontinue insulin and to seek professional advice early in the course of the illness Case 4: Neuropathy AF is a 74 y/o female with Type 2 DM. She has neuropathy in her feet and was recently started on Lantus 10 units at bedtime. She is complaining that the burning in her feet has gotten worse since she started taking Lantus. She didn’t take the insulin last night for that reason. What do you advise? Circulation Comparison Molasses vs. Water Diabetes Mellitus Ibrahim Sales, Pharm.D. Assistant Professor of Clinical Pharmacy King Saud University isales@ksu.edu.sa