Applied Behavior Analysis
advertisement

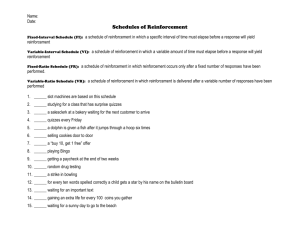
Applied Behavior Analysis: Concepts, Principles and Methodology for the Brain Injury Practitioner to address the challenges of neurobehavioral issues in post-acute rehabilitation. Presenters: Chris Schaub, MscEd, BCBA Christina Peters, MscEd, BCBA, CBIS Overview & Objectives This half day workshop will provide: 1. To provide an overview of behavior analytic philosophy, principles and procedures toward developing effective interventions for specific target behaviors. 2. To present broad guidelines for developing and implementing comprehensive, interdisciplinary treatment programs for individuals with intensive neurobehavioral needs, including aggression, elopement, resistance, dual diagnosis, etc... 3. To share information that will help clinicians, staff, funders and administrators within the field identify and prioritize treatment plan elements that are essential to integrated, comprehensive neurobehavioral rehabilitation. Clients we serve… • Are difficult to place following acute rehabilitation – Medical complexity results in and/or is complicated by neurobehavioral instability • Medication issues • Sleep disturbances • Vestibular Disorders • Chronic Pain • Unresolved issues with bowel and bladder function • Unresolved eating and hydration issues • Post-traumatic confusion Clients we serve… • Exhibit emergent, persistent or pre-existing issues that prohibit progress (at any level) – At risk behaviors and/or safety concerns secondary to awareness deficits • Refusal & Resistance • Substance Abuse • Aggression • Threats & Violence • Sexual disinhibition • Pre-existing MH issues Clients we serve… • Have been discharged to the home environment and are too challenging for the family/caregiver – – – – Programming not available, limited and/or lacks integration Behavioral stability is questionable Change in behavioral patterns Change in medical stability impacts mood, behavior, cognition, etc… – Acute/emergent destabilization – Danger to community/family or self Post-Acute Neurobehavioral Rehabilitation at ReMed Neurobehavioral Sequelae • • • • • • • • • Medical complexity PTA Persistent cognitive impairment Acute medical/behavioral instability Resistance/Refusal Threats & Aggression Wandering & Elopement Substance abuse Co-occurring issues Interdisciplinary Team • Physiatry, Neuropsychiatry, Neurology & Consultants • Nursing • PT • OT • SLP • Psychology & Neuropsychology • D&A Counselor • Behavior Analyst • TR Evolution of Neurobehavioral Programming • Admission & Stabilization – Priority is typically medical and/or behavioral stability – Frequently precedes comprehensive rehabilitation efforts • Evaluation & Treatment – Interdisciplinary team completes evaluations, identifies goal areas and establishes treatment plan – Integrated programming and rehabilitation supports stability and progress in key areas • Generalization & Maintenance – Trials, education and training support efforts to expand programming and maximize independence – Consider transitions and/or discharge planning Importance of Philosophy • Guides interdisciplinary team in comprehensive assessment and treatment efforts • Provides clinical framework for prioritizing issues • Enables treatment programming to be highly individualized • Promotes integration at all levels and areas of programming Neurobehavioral Philosophy: 3 Keys to Stability & Success Establish Medical Stability Promote Behavior Stability & Cognitive Enhancement Comprehensive & Integrated Programming Develop Stable Activity Plan Establish Medical Stability Promote Behavior Stability Develop Stable Activity Plan Sources of Medical Instability & Interdisciplinary Involvement Issue(s) • Pain • Vestibular • Medication regiment and compliance • Poor Sleep • Bowel/Bladder Incontinence • Drug and Alcohol Use • Acute, unresolved or pre-existing medical issues/conditions Team Member(s) • • • • • • • • Physiatrist Neuropsychiatrist Neurologist Consultants Rehab Nursing PT D&A BA Establish Medical Stability Promote Behavior Stability Develop Stable Activity Plan Characteristics of Behavior Instability & Interdisciplinary Involvement Issue(s) • • • • • • Confusion/Disorientation Poor/Limited Awareness Refusal/Resistance Mood Instability Threatening/Demanding Verbal &/or Physical Aggression • Property Destruction • Elopement • Substance Use Team Member(s) • • • • • • • • Neuropsychiatrist Neuropsychology Psychology BA D&A OT PT TR Establish Medical Stability Promote Behavior Stability Develop Stable Activity Plan Features of an Unstable Activity Plan & Interdisciplinary Involvement Issue(s) • Poor follow through &/or initiation • Limited choice • Imbalance of reinforcement availability/potency with regard to preferred activities • Inattention to risks associated with competing reinforcers or inaccessibility of support Team Member(s) • • • • • • • TR OT PT Psych BA Cog D&A The Analysis of Behavior: Key Points •Definition of behavior includes thinking, saying and doing •Behavior occurs, interacts with the environment and produces consequences •Darwinian-like model wherein behaviors are selected by the environment •The goal of behavior analysis is to enable prediction and change of behavior Two Types of Learning Operant Respondent • Concerned with environmental events that precede target responses. • Concerned with environmental events that follow the responses (its consequence) •S •R S R Operant Conditioning • But as you probably already noticed, we do not simply react to stimuli in the environment. • Based on our history, we also act in ways that affect or change the environment. • Operant conditioning is a training or learning process by which the consequence of a response affects the likelihood that the individual will produce that response again. The Three and Four Term Contingency The familiar…. 3 Term A→B→C The more precise… 4 Term _ D +/ E.O. → S → R → S The Four Term Contingency Establishing Operation: Any change in the environment that alters the effectiveness of some stimulus or event as a reinforcer. Discriminative Stimulus: An event or stimulus that precedes a response and sets the occasion for the behavior to occur. Response/Behavior: "If a dead man can do it, it ain't behavior. And if a dead man can't do it, then it is behavior" Stimulus: Any event that changes the probability of a response when presented after it: S+ refers to a stimulus that increases the probability of a behavior occurring, and S_ refers to a stimulus that decreases the probability of a behavior occurring…but more on that later. Reinforcement Reinforcement refers to any process that increases the likelihood that a particular response will occur again in the future. Positive Reinforcement occurs when the arrival/delivery of some stimulus following a response makes that response more likely to occur in the future. Negative Reinforcement occurs when the removal of a stimulus following a response make that response more likely to occur. Punishment Punishment refers to any process that decreases the likelihood that a particular response will occur again in the future. Positive Punishment occurs when the arrival/delivery of some stimulus decreases the likelihood that the response will occur again. Negative Punishment occurs when the removal of some stimulus decreases the likelihood that the response will occur again. Positive R E I N F O R C E M E N T P U N I S H M E N T A stimulus is added such that the likelihood of the behavior increases. A stimulus is added such that the likelihood of the behavior decreases. Negative A stimulus is removed such that the likelihood of the behavior increases. A stimulus is removed such that the likelihood of the behavior decreases. R E I N F O R C E M E N T P U N I S H M E N T Positive Negative A day laborer is paid after 8 hours of work, as a result they return the next day. After hitting the snooze button the alarm goes off, as a result the snooze button is used more in the future. A pink slip is issued to the late employee, as a result the employee begins to come to work late less often. A fine is issued to a driver for speeding, as a result the driver speeds less frequently. Function • Function is the behavior analytic term that refers to “why" an individual exhibits a certain behavior; specifically, it refers to those consequences that maintain the behavior. • Often, an individual will display a number of behaviors that may differ in topography but share a similar function; these are referred to as Functional Classes of Behavior. • All operant behavior occurs within some context, and understanding this context is key to modifying any behavior. Schedules of Reinforcement • Extinction: A particular response never produces a reinforcer. • Continuous Reinforcement: A particular response always produces a reinforcer (1:1). • Intermittent Reinforcement: A particular response sometimes produces a reinforcer. Continuous Reinforcement • Produces less variability in topography of behavior. • Utilized to promote acquisition of behavior • Behavior is highly sensitive to extinction • Think piece work and soda machines Intermittent Reinforcement • Produces greater variability in topography of behavior. • Utilized to promote generalization and maintenance of behavior • Behavior is highly resistant to extinction • Think hourly pay and slot machines Why Do We Need to Know About Schedules of Reinforcement? • In order to understand what is maintaining a particular behavior we not only need to look at the function of that behavior, but also the schedule on which it is being reinforced or maintained. • Behaviors within the same functional class can be sensitive to concurrent schedules of reinforcement, making analysis more critical. • Attempting to intervene without this knowledge could result in danger to client or others. Establish Medical Stability Promote Behavior Stability Develop Stable Activity Plan Establish Medical Stability: Principles and Programming To Be Considered Principles Programming • Establishing operations • Crisis Plan • Antecedents • Structured routine • Acknowledge limited • Data collection efficacy of consequencebased programming • Identify and define target behaviors • Establish criteria for stability • Prioritize behaviors and expectations Establish Medical Stability Promote Behavior Stability Develop Stable Activity Plan Promote Behavior Stability: Principles and Programming To Be Considered Principles Programming • Function • Preference Assessment • Reinforcement • Functional Analysis • Contingencies, Schedules & Potency • Specific procedures & tools; • NCR, DR and EXT • Extinction • Shaping, chaining and fading • Generalization • Criteria Checklists & Phase Plans • Maintenance • Data-based decisions Establish Medical Stability Promote Behavior Stability Develop Stable Activity Plan Develop Stable Activity Plan: Principles and Programming To Be Considered • • • • • • Principles Schedules of reinforcement Potency of reinforcers Differential reinforcement Generalization Maintenance Premack Principle • • • • Programming Pacing Continue data-based decision making Refine and work towards criteria for stability and safety Promote generalization and maintenance of skills Continuum-based Neurobehavioral Programming • Critical questions often are at the core of the post-acute process • Must consider and address challenging and complex sequelae across treatment areas • Must take into account funding and available time and resources • Need to answer questions in clear and accurate manner Building Towards Independence • Identify component skills necessary • Determine how best to promote acquisition • Consider combinations of skills • Generalization and maintenance • Use multiple differential reinforcement contingencies Sample Data Collection Tool #1 “Phase Plan” Sample Data Collection Tool #2 “Criteria Checklist” Sample Data Collection Tool #3 “Individualized Daily Schedule” Promoting Movement Towards Less Restrictive Setting • Work begins at STIRS with the interdisciplinary team. • Team supports client to participate in the plan to maximize stability and independence • Less restrictive placement options are explored and trialed, which can include transitioning within ReMed’s continuum or beyond • The plan ultimately guides readiness-based decisions or conclusions by providing objective behavior data • The structure of the plan mitigates issues related to awareness deficits in such a manner that they are not necessarily a barrier to progress Sample Data Collection Tool #4 “MacroTracker” Case Study #1 ‘Sara’ “Sara” Psycho-Social Profile • 29 years post injury, injured at 15 years old. • History of admissions and discharges to/from various inpatient facilities secondary to behavioral dyscontrol. • Use of ‘medication interventions’ and inpatient admissions to stabilize aggressive behaviors. • Risperidone introduced with significant negative side effects. • Admitting from home where care giving responsibilities were shared between family, friends and one hired caregiver secondary to burnout. • Family states that they are prepared to take her back home following admission but only if things are different. “Sara” Clinical Profile – Aggression (hitting & kicking caregivers and family – Threatening – Sexually Inappropriate Behavior – Mood instability – Impulsivity – Residual Cognitive Impairment – Poor Self Awareness – Bowel and Bladder Incontinence – Confusion/Disorientation – Resistance/Refusal of Medications – Non-reality based statements accompanied with emotionality. – Falls Risk – Sedation secondary to medication; decreased mobility, poor posture, drooling, reduced swallow response. “Sara” Referral Questions & Client Goals • Referral Questions – Why haven’t other attempts to stabilize and return to home worked? – Can Generalization and Maintenance be achieved? If so, how? – Can there be a protocol be for managing future episodes of destabilization so that last resort interventions can be avoided? • Client Goals – – – – Return home Be more independent Access the community more often Relationship Case Study #2 ‘Melissa’ “Melissa” Psycho-Social Profile • 10 years post injury • History of treatment non-compliance, psychiatric admissions, several arrests for possession • Multiple admissions previously to residential and outpatient brain injury programs • Admitting from apartment situation; currently exhibiting issues with relapse, mood instability, refusal/resistance to treatment; high risk behavior • Accessing community but no work/volunteer situation, not attending fellowship/AA, limited social network and/or leisure options • Family not prepared to have them live at home under any circumstances “Melissa” Clinical Profile – Executive dysfunction • Impulsivity • Impaired judgment and problem solving • Poor frustration tolerance – – – – – – – Poor awareness Mood instability (lability, history of depression) History of Substance Abuse Verbal & Physical Aggression, Property Destruction Sexually Inappropriate/At-Risk Behavior Elopement Risk SIB (cutting, burning) “Melissa” Referral Questions & Client Goals • Referral Questions/Objectives – Are you willing/able to provide treatment ? – Promote and establish safety – Encourage treatment participation – Optimize independence • Melissa’s Goals – – – – Live independently Work competitively Drive Relationship